To properly sterilize nitrous oxide equipment, you’ll need to follow a systematic multi-step process. Start with thorough inspection and pre-cleaning using approved enzymatic detergents. Next, utilize ultrasonic cleaning to remove debris, followed by complete drying and verification of component integrity. Apply terminal sterilization methods while maintaining NO2 concentrations at 1% of ambient pressure. You’ll also need to implement regular monitoring and documentation protocols – there’s much more to ensuring complete sterility and safety compliance.
Understanding NO2 Sterilization Components

Nitrogen dioxide (NO₂) sterilization represents a vital advancement in medical equipment sterilization, operating through a precise gas-phase mechanism at room temperature and atmospheric pressure. You’ll find this method exceptionally effective as it requires only 1% concentration of ambient pressure, ensuring ideal gas composition optimization while minimizing chemical residue risks. Unlike traditional methods which often face capacity constraints, this approach provides terminal sterilization for over 20 billion medical devices annually. The process achieves a log-linear reduction in microbial populations as exposure time increases. The system’s efficiency stems from its ability to maintain gaseous form without condensation, allowing for superior penetration into complex instrument geometries. This method has proven particularly valuable in low-resource environments, where access to traditional sterilization equipment may be limited. You’ll benefit from efficient aeration techniques that enable rapid post-sterilization dissipation, greatly reducing equipment downtime. The process delivers consistent microbial reduction, achieving sterility assurance levels within 20-40 minutes for typical devices. When you’re implementing NO₂ sterilization, you can rely on established validation protocols that meet regulatory requirements for terminal sterilization in medical settings.
Pre-Sterilization Equipment Preparation
Before sterilizing nitrous oxide equipment, you’ll need to conduct a thorough inspection of all components, checking for wear, damage, or debris that could compromise the sterilization process. Your cleaning protocol should begin with disassembling the equipment and washing all parts with an approved enzymatic detergent, followed by ultrasonic cleaning when appropriate for specific components. Using sound waves to remove bioburden helps ensure thorough decontamination of hard-to-reach areas. After cleaning, you must completely dry all equipment using approved methods and verify that no moisture remains trapped in hoses or internal chambers before proceeding with sterilization. All staff members handling the equipment must wear PPE to ensure safety during the preparation process.
Equipment Inspection Guidelines
Proper equipment inspection serves as the cornerstone of safe nitrous oxide administration in therapeutic settings. You’ll need to establish periodic visual inspections and proactive maintenance schedules to guarantee system integrity. Cross-infection risks can arise from inadequate equipment cleaning between patients. Following manufacturer Instructions for Use is legally required and essential for proper maintenance and cleaning procedures.
Start by examining rubber hoses and nasal hoods for holes or tears. Check that all component connections are secure to maintain gas flow integrity, and verify that your alarm systems for nitrous/oxygen monitoring are functioning correctly. Don’t forget to inspect odor-absorbing filters for signs of saturation. Regular inspections should maintain N₂O levels at below 25 ppm through active scavenging.
For single-use components, verify they’re undamaged before use and properly discard them afterward. When inspecting the system, you’ll need to confirm that the scavenger system operates effectively and test pressure rates in delivery lines. Use soapy water during monthly leak checks to identify any connection issues.
Cleaning Protocol Steps
When preparing nitrous oxide equipment for sterilization, you’ll need to follow a systematic cleaning protocol that removes all contaminants and bioburden. Start by washing all components with a mild, neutral pH detergent and warm water while monitoring airflow parameters to guarantee thorough cleaning.
Key steps in the cleaning process include:
- Pre-soak equipment in approved detergent solutions if immediate reprocessing isn’t possible
- Use ultrasonic cleaners or automated instrument washers with reprocessing indicators to verify cleaning efficacy
- Remove all chemical residues through thorough rinsing before proceeding to sterilization
Always wear protective gear and use long-handled brushes during manual cleaning. Don’t use household cleaners, as they can damage the equipment. Instead, select oxygen-compatible cleaning solutions that meet EIGA Doc 33 or ISO 23208 standards, maintaining contamination levels below 500 mg/m².
Essential Safety Protocols and Guidelines

Safety protocols serve as the foundation for maintaining sterile nitrous oxide equipment in therapeutic settings. You’ll need to implement strict staff training requirements and conduct regular regulatory compliance reviews to guarantee proper sterilization procedures. The FDA’s most recent sterilization guidance updates in January 2024 provide critical new standards for medical device sterilization.
Always follow FDA-approved disinfection methods, using alkaline glutaraldehyde for rubber nasal masks and avoiding prohibited techniques like cold or dry sterilizers. When sterilizing equipment, you must choose between steam autoclaving for heat-resistant materials or ethylene oxide (EtO) for sensitive components. Remember to properly prepare instruments by removing all residues and confirming material compatibility before sterilization. Improper cleaning of instruments can lead to sterilization failure by preventing sterilizing agents from reaching all surfaces effectively.
You’ll need to maintain detailed documentation of sterilization cycles and instrument tracking. Don’t forget to monitor EtO emissions according to EPA requirements and ensure all sterilized items remain wrapped until use to prevent contamination.
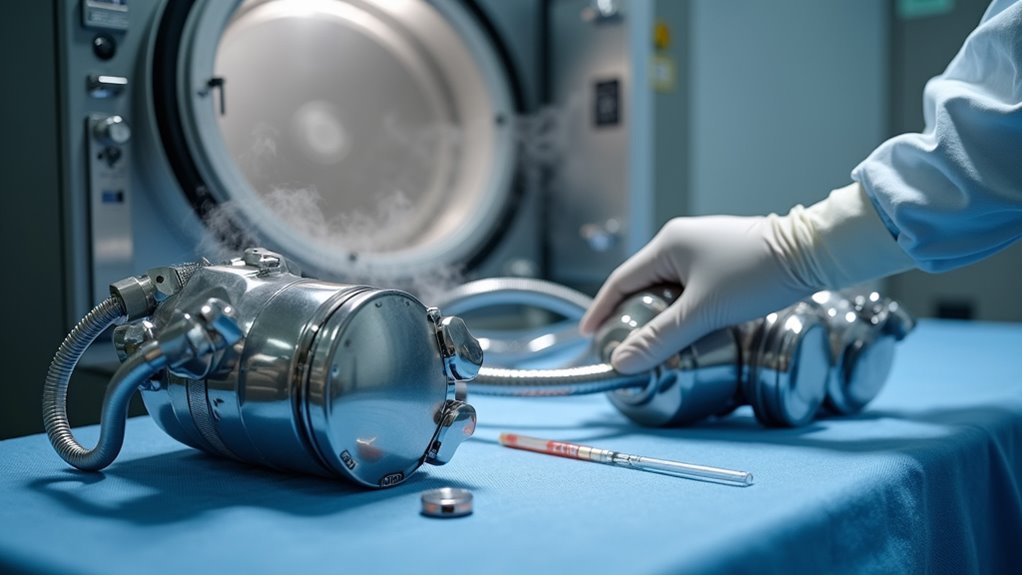
Step-by-Step Sterilization Process
The sterilization process begins with precise chamber preparation and environmental control measures. You’ll need to evacuate air from the chamber and introduce nitrogen dioxide at concentrations below 21 mg/L while maintaining ambient pressure through humidified air addition.
- Monitor sterilant degradation factors including temperature, humidity, and pressure, to guarantee optimal gas-phase consistency
- Preserve exposure times between 20-40 minutes while conducting nitrogen dioxide monitoring throughout the cycle
- Complete a rapid aeration phase post-cycle, confirming safe residual levels before handling equipment
The process concludes with validation using biological indicators, specifically testing with Geobacillus stearothermophilus. You’ll need to document all cycle parameters and microbial reduction data for regulatory compliance. In addition, the gas-phase operation at room temperature preserves heat-sensitive materials while achieving a sterility assurance level of 10^-6.
Quality Control and Validation Methods
Quality assurance in nitrous oxide sterilization demands rigorous validation protocols and analytical testing methods. You’ll need to conduct sterility testing in controlled environments at 25°C and 60% relative humidity, using gas chromatography with electron capture for precise analysis. Your sampling methodologies must account for both active and passive monitoring techniques, adjusting for humidity variations that can affect results. Medical facilities must maintain thorough batch records and detailed documentation for every sterilization process.
Implement strict record-keeping protocols that document contaminant levels, batch validation, and sterilization parameters. You’ll need to maintain Certificates of Analysis for each batch, ensuring 99.99% purity for medical-grade nitrous oxide. Store all sterilized components in their original packaging until use, and verify compliance with the manufacturer’s guidelines for dosage, temperature, and time specifications. Follow FDA GMP standards to maintain complete traceability of all sterilization processes and test results.
Post-Sterilization Equipment Handling
Proper post-sterilization handling of nitrous oxide equipment requires systematic adherence to contamination control protocols. After sterilization, you’ll need to maintain sterile chamber storage conditions and update patient traceability records to guarantee safety and compliance.
Key practices for maintaining sterility include:
- Keep sterilized items in sealed pouches until immediate use, avoiding premature opening or hand contact
- Position equipment away from chamber walls during storage to prevent chemical residue exposure
- Verify complete internal and external drying before packaging to avert microbial growth
When handling post-sterilized components, always inspect packaging integrity before use. Document each sterilized item’s batch number and storage location in your traceability system. If you notice any moisture, damage, or compromise to sterile barriers, reprocess the items immediately following manufacturer guidelines. Using an enzymatic detergent solution for cleaning components before sterilization helps ensure thorough removal of contaminants.
Proper Storage and Maintenance Practices
Maintaining safe and effective nitrous oxide equipment storage requires systematic management across multiple control points. You’ll need to implement restricted access protocols while ensuring proper segregation of used and new equipment.
Store your cylinders upright in secured, ventilated areas away from heat sources and direct sunlight. You’ll want to monitor cylinder weights regularly and conduct controlled substance reconciliation through detailed audit trails. Keep your components in sterilization packaging until they’re needed, and track usage patterns to maintain adequate inventory levels.
For system maintenance, always depressurize equipment before repairs and follow gas service change procedures precisely. When storing sterilized components, maintain proper separation between used and clean items. Remember to dispose of single-use items appropriately and replace any components that have exceeded their recommended sterilization cycles.
Troubleshooting Common Sterilization Issues
When troubleshooting sterilization failures, you’ll need to address moisture interference that prevents proper gas penetration and creates conditions for microbial regrowth. Your equipment load configuration must maintain adequate spacing between components while ensuring proper orientation for complete sterilant exposure throughout the chamber. You’ll also need to verify consistent gas distribution by monitoring pressure gauges and flow indicators during the sterilization cycle to prevent “cold spots” where inadequate sterilization may occur.
Moisture-Related Process Failures
Moisture-related failures during sterilization can compromise the safety and efficacy of nitrous oxide delivery systems. You’ll need to carefully monitor cycle time requirements and temperature control standards while addressing these critical moisture concerns. Improper cleaning of components before sterilization can lead to residue buildup that traps moisture and prevents effective sterilization.
- Guarantee components are completely dry before wrapping, as trapped moisture can interfere with steam penetration and create breeding grounds for microorganisms
- Configure your sterilization chamber to prevent equipment from touching walls and maintain proper airflow, reducing the risk of moisture accumulation
- Implement validated packaging protocols using steam-permeable materials that maintain sterility while allowing proper moisture evaporation
When you detect moisture issues, immediately adjust your drying procedures and verify sterilizer compatibility. Only use validated steam sterilizers with moisture control mechanisms, and always follow manufacturer-specific protocols for drying times and storage conditions. Document all moisture-related interventions for quality assurance.
Equipment Load Configuration Issues
Proper load configuration directly impacts the success of nitrous oxide equipment sterilization. When you’re loading sterilization chambers, avoid tight packing that creates uneven exposure zones and blocks sterilizing agents from reaching all surfaces. Don’t exceed the manufacturer’s specified capacity limits, as this leads to inadequate load monitoring and compromised disinfection. Regular spore testing weekly helps verify successful sterilization cycles and equipment performance.
You’ll need to rotate instruments during loading to optimize exposure and follow the manufacturer’s recommended configurations. Always use validated sterilization packaging with appropriate spacing between wrapped items to guarantee proper steam circulation. Place equipment on the provided loading trays or pegs as specified in the guidelines. If you’re using cassettes, arrange them to prevent jamming that could obstruct uniform penetration of sterilizing agents. Remember, skipping these critical setup steps can result in failed sterilization cycles.
Incomplete Gas Distribution Problems
A systematic approach to troubleshooting incomplete gas distribution starts with identifying the root mechanical causes. Flow rate inconsistencies and residual gas accumulation often stem from equipment malfunctions that you’ll need to address promptly.
- Check for stuck valves and clogged filters that restrict proper gas flow, leading to uneven distribution throughout your delivery system
- Inspect all connections between components, paying special attention to worn O-rings that can create pressure inconsistencies and compromise gas delivery
- Monitor your scavenging system’s pressure levels to prevent gas buildup, ensuring there’s no tubing obstruction or improper setup
You’ll need to verify that your cylinder pump readings are accurate and that your pipeline system isn’t experiencing pressure fluctuations. Regular preventative maintenance testing should be performed to identify potential leaks and system failures before they occur. Address any mechanical issues immediately to maintain ideal gas distribution and patient safety.
Frequently Asked Questions
How Often Should Sterilization Filters Be Replaced in Nitrous Oxide Delivery Systems?
You’ll need to replace sterilization filters in nitrous oxide delivery systems at multiple intervals based on specific triggers. Follow manufacturer guidelines for a minimum of 6-month replacements, but increase frequency with high patient volume. You must replace filters immediately after contamination exposure or failed sterilization verification procedures. Always swap filters during annual system overhauls and after repairs. Don’t forget to document each filter replacement to maintain compliance records.
Can Sterilized Nitrous Oxide Equipment Be Transported Between Different Therapy Facilities?
You can transport sterilized nitrous oxide equipment between facilities, but you’ll need to meet strict portable storage requirements and sterilization verification methods. You must use airtight packaging, maintain proper temperature control, and document all sterilization procedures. You’ll need to follow CDC guidelines, verify equipment integrity upon arrival, and guarantee that both facilities approve the transfer. Don’t transport single-use components like disposable nasal masks, and always check the manufacturer’s instructions beforehand.
What’s the Shelf Life of Sterilized Nitrous Oxide Equipment Components?
You’ll find that sterilized nitrous oxide components don’t have a fixed shelf life. Once you open the sterile packaging, you must use the equipment immediately. Storage temperature and shelf life variability depend on your facility’s controlled environment conditions. You’ll need to re-sterilize reusable components before each use, regardless of storage duration. Remember, you can’t preserve sterility after opening; environmental exposure automatically invalidates the sterilization status.
Does Extreme Weather Affect the NO2 Sterilization Process Effectiveness?
You’ll find that NO₂ sterilization remains largely unaffected by extreme weather conditions due to its controlled chamber environment. Temperature variations outside the system don’t materially impact sterility maintenance because the process operates at room temperature in sealed chambers with regulated humidity. While you should monitor your facility’s power supply during severe weather, the sterilization effectiveness stays consistent thanks to automated controls and internal environment regulation systems.
Are There Specific Humidity Requirements for Storing Sterilized Nitrous Oxide Equipment?
You’ll need to maintain ambient humidity levels between 30-60% for storing sterilized N2O equipment. It’s critical to avoid temperature fluctuations that could cause condensation. You should monitor your storage area daily using a hygrometer and guarantee proper ventilation. Don’t store equipment in basements or damp areas where moisture can accumulate. Keep sterilized components in their sealed packaging until use, and implement a monitoring system to track environmental conditions consistently.