Cognitive Behavioral Therapy (CBT) fundamentally operates on the principle that your thoughts, emotions, and behaviors are interconnected in what’s called the cognitive triangle. This connection means negative thinking patterns directly influence how you feel and act. By identifying and challenging unhelpful thoughts and core beliefs, you can break destructive cycles and develop healthier response patterns. CBT’s structured, present-focused approach empowers you with practical skills to transform your thinking a process backed by decades of compelling neurobiological and clinical evidence.
The Cognitive Triangle: Understanding the Thought-Emotion-Behavior Connection

The Cognitive Triangle represents one of the foundational frameworks in Cognitive Behavioral Therapy, illustrating how thoughts, emotions, and behaviors continuously influence one another in a cyclical pattern.
When you experience situational triggers, your immediate thoughts often automatic and potentially involving cognitive distortions directly shape your emotional responses. These emotions, in turn, drive your behavioral responses, creating feedback loops that can either reinforce negative cycles or build positive reinforcement.
Developing self-awareness of these connections empowers you to intervene at any point in the triangle. CBT efficacy studies have demonstrated that approximately 80% of adults benefit from cognitive therapy interventions targeting these interconnected elements. The therapy remains goal-oriented throughout the treatment process, helping clients develop practical skills they can apply independently. By practicing thought reframing, emotional regulation, and intentional behavior modification, you can break destructive patterns.
Without intervention, the triangle becomes a vicious cycle that perpetuates negative patterns in daily life.
This understanding forms the basis for effective coping strategies, helping you transform negative cycles into constructive ones, regardless of which component you initially target.
Core Beliefs and Their Impact on Mental Health
While thoughts and behaviors fluctuate from moment to moment, core beliefs operate as the foundational architecture of your cognitive framework, profoundly shaping your perception of reality.
These deeply held convictions, largely formed through childhood experiences, act as filters for all emotional processing and subsequent reactions.
Negative core beliefs can have a devastating impact on mental health, manifesting as self-sabotage, diminished self-worth, and persistent anxiety or depression. Core beliefs play a significant role in various mental health disorders, particularly in how symptoms develop and persist.
Core negative beliefs hijack our self-perception, fueling destructive patterns of self-sabotage and emotional distress.
When you believe you’re fundamentally flawed or unlovable, you unconsciously seek evidence that confirms these distortions. This perpetuates a cycle where experiences contradicting negative beliefs are often cognitively filtered out.
Cognitive restructuring in CBT helps you identify and challenge these unhelpful beliefs, gradually replacing them with more balanced, adaptive beliefs. Dr. Aaron Beck’s revolutionary approach established that changing these thought patterns directly improves emotional well-being.
This transformation process is essential for sustainable mental health improvement and breaking free from self-limiting patterns.
Evidence-Based Foundations of CBT’s Effectiveness

CBT’s effectiveness rests on decades of solid empirical research, with meta-analyses consistently demonstrating significant symptom reduction across different mental health conditions compared to control groups.
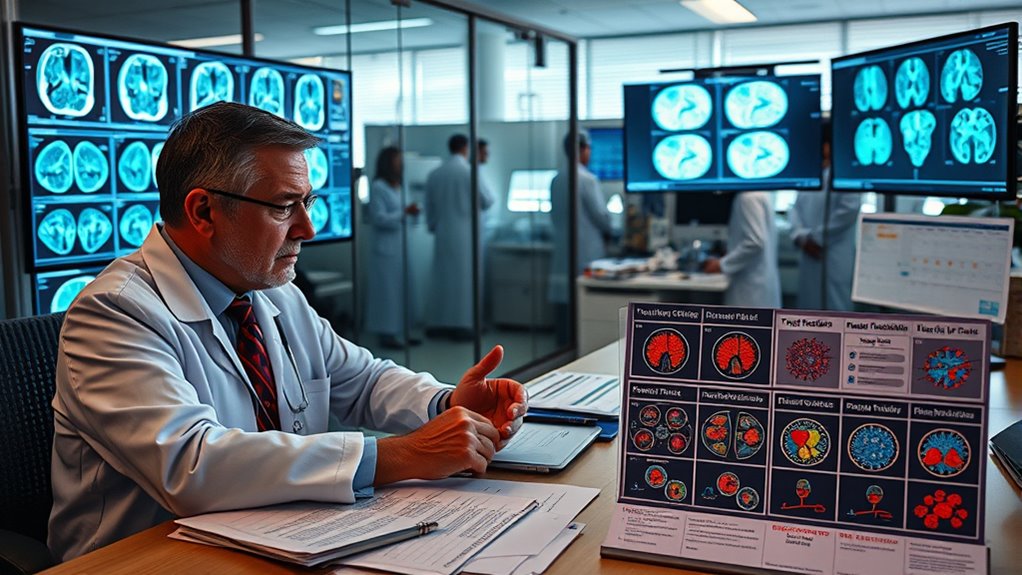
You’ll find strong neurobiological evidence supporting CBT’s mechanisms, including studies showing changes in brain activity patterns following successful treatment.
This evidence-based approach has established CBT as a primary treatment recommendation in clinical guidelines worldwide, with particularly strong outcomes for anxiety disorders, depression, and PTSD. A recent study published in The Lancet Psychiatry demonstrated that CBT provides long-term benefits for patients with depression, especially those who did not fully respond to antidepressants alone. The structured techniques employed in CBT effectively transform thought patterns and behaviors, which contributes to its widespread success as a therapeutic intervention. Current research recognizes CBT as having the most supporting evidence among all psychological therapies for improving health-related quality of life.
Empirical Research Outcomes
Extensive research spanning decades has firmly established Cognitive Behavioral Therapy as one of psychology’s most empirically validated treatment approaches. The empirical efficacy of CBT is demonstrated across numerous mental health conditions, with therapeutic outcomes consistently showing strong and lasting effects.
- Large effect sizes for both depression and anxiety disorders, with CBT often outperforming antidepressant medications.
- Proven effectiveness across age ranges, from very young children (3-6 years) to adults with diverse conditions.
- Superior long-term outcomes, with patients showing lower relapse rates compared to medication-only treatments.
- Cost-effectiveness particularly notable in mindfulness-based CBT for depression relapse prevention.
Meta-analyses have consistently shown that CBT is more effective than psychodynamic therapy and comparable to other therapeutic approaches for treating anxiety and depression.
While CBT’s effectiveness differs by condition and delivery method, the evidence overwhelmingly supports its central role in contemporary mental health treatment, especially when customized to specific disorders.
Meta-Analysis Support Data
The empirical foundation of Cognitive Behavioral Therapy rests upon an impressive body of meta-analytic research that substantiates its effectiveness across diverse psychological conditions. A thorough review identified 269 meta-analytic studies, with strongest support for anxiety, somatoform disorders, bulimia, anger, and stress.
Meta-analysis findings reveal moderate to large effects compared to control conditions (g=0.79), with benefits maintained at follow-up periods of 6-12 months.
You’ll find CBT outperforms other psychotherapies and shows greater long-term effectiveness than pharmacotherapy at one-year follow-up (g=0.34).
Treatment efficacy extends beyond mental health to physical conditions, demonstrating medium effect sizes for chronic pain and fatigue. Recent research demonstrates that ultra-complex CBT shows the highest effectiveness in reducing depression with standardized mean differences of -1.45. Recent evidence shows CBT significantly improves outcomes for patients with bipolar disorder when used as an adjunctive therapy to medication.
CBT also proves effective for children and adolescents, with particularly strong outcomes for youth anxiety disorders.
Neurobiological Change Evidence
Modern neuroscience has dramatically expanded our understanding of how cognitive behavioral therapy creates measurable changes in brain structure and function. Research demonstrates CBT’s ability to produce significant neurotransmitter modulation and brain structure changes visible through sophisticated imaging techniques.
Key neurobiological findings include:
- Decreased amygdala activation and volume following CBT treatment, correlating with reduced anxiety responses
- Normalized prefrontal cortex activity in depression patients, improving cognitive control over emotions
- Improved neurochemical concentrations in the OFC, ACC, and striatum regions following therapeutic interventions
- Formation of new neural pathways as you practice CBT techniques, demonstrating the brain’s remarkable neuroplasticity
Studies show approximately 70% of OCD patients respond positively to CBT treatment, with many exhibiting lower relapse rates compared to those treated with pharmacotherapy alone.
These biological changes confirm that CBT doesn’t just alter thoughts and behaviors it physically rewires your brain, creating lasting neurological improvements that support recovery from psychological distress. Meta-analyses of neuroimaging studies reveal consistent changes in the default mode network following effective CBT interventions across various psychiatric disorders. The intervention’s effectiveness is based on the fundamental principle that cognitions influence emotions and behaviors, providing the theoretical foundation for therapeutic approaches.
Challenging Cognitive Distortions and Automatic Thoughts

Five fundamental patterns of distorted thinking lie at the heart of cognitive behavioral therapy practice. These include all-or-nothing thinking, overgeneralization, mental filtering, catastrophizing, and personalization.
These exaggerated thought patterns, formed during childhood, can greatly worsen symptoms of anxiety and depression.
Through automatic thought identification, you’ll learn to recognize those immediate, unquestioned responses that trigger emotional reactions. Mental flexibility in thought can help break these rigid thinking patterns and allow for more balanced interpretations. Cognitive reframing techniques like Socratic questioning and examining evidence help you critically assess these thoughts.
By documenting your thoughts using structured records, you’ll develop awareness of recurring patterns.
The restructuring process involves identifying distortions, evaluating evidence, and generating balanced alternatives. Cognitive therapy emphasizes that thought modification leads to improved mental health outcomes. Maintaining a growth mindset rather than a fixed one is essential in cognitive restructuring, as replacing entrenched negative thought patterns requires persistence. As you practice challenging these distortions, you’ll experience improved emotional regulation, improved problem-solving abilities, and greater resilience when facing life’s challenges.
The Present-Focused Nature of CBT Intervention
CBT’s effectiveness stems from its focus on your current challenges rather than extensive exploration of your past.
You’ll develop practical skills to address immediate thought patterns and behaviors that contribute to your distress today.
This present-centered approach enables you to make meaningful changes in your daily life while building sustainable coping strategies for long-term wellbeing.
The therapy’s structured approach allows for clear goal-setting and measurable progress throughout your treatment journey.
The therapy incorporates Socratic questioning to help you identify and modify negative thinking patterns that affect your emotions and behaviors.
Why Now Matters
While many therapeutic approaches investigate a client’s past experiences, cognitive behavioral therapy distinguishes itself by placing a deliberate focus on the present moment.
CBT prioritizes addressing your current challenges rather than extensively analyzing childhood events, allowing you to take immediate action towards meaningful change.
This present-focused approach delivers several key benefits:
- Provides rapid symptom relief within a relatively short timeframe (typically 12-16 weeks)
- Interrupts negative thought patterns as they occur in real-time
- Promotes behavioral activation to overcome current avoidance patterns
- Builds self-efficacy by equipping you with practical coping skills
Skills Over History
Rather than dwelling on past experiences that can’t be changed, CBT equips you with practical skills to address your current challenges head-on. The approach prioritizes solving immediate problems through active skill development, focusing on how your thoughts and behaviors affect you today.
Unlike therapies that extensively investigate historical context, CBT emphasizes skill evolution through collaborative practice. You’ll work with your therapist to identify unhelpful thinking patterns and develop concrete techniques to manage them.
This present-focused approach means your treatment can often be completed within 6-14 sessions.
CBT’s effectiveness comes from teaching you to become your own therapist. Through homework assignments and regular practice outside sessions, you’ll build confidence in applying these skills independently, creating sustainable change without extensive historical analysis.
Behavioral Activation as a Catalyst for Positive Change
Behavioral activation stands as one of the most powerful components within cognitive behavioral therapy, functioning as a catalyst that can transform negative psychological patterns into positive change. This approach systematically breaks the cycle of avoidance and withdrawal through structured behavioral strategies and activity scheduling that gradually reintroduce positive experiences into your life.
The effectiveness of behavioral activation stems from four key principles:
- Engagement in rewarding activities directly improves mood, regardless of thought patterns
- Scheduled activities build momentum that overcomes initial motivation barriers
- Progressive difficulty increases confidence through successful experiences
- Activity selection based on personal values guarantees sustainable engagement
Research shows behavioral activation can be as effective as medication for depression, making it a cornerstone intervention that builds psychological resilience through action rather than insight alone.
The Collaborative Therapeutic Alliance in CBT
The collaborative therapeutic alliance in CBT represents far more than a mere backdrop for technical interventions it forms the essential foundation upon which all effective cognitive behavioral therapy is built. Research consistently identifies this alliance as a significant predictor of treatment outcomes across numerous disorders.
| Alliance Component | Alliance Building Techniques |
|---|---|
| Goal Agreement | Socratic questioning to develop shared objectives |
| Task Collaboration | Regular alliance assessment and feedback |
| Emotional Bond | Tailoring communication to individual needs |
Successful therapist-client dynamics balance structured intervention with genuine empathy, creating space where clients feel both supported and challenged. When you encounter ruptures in the therapeutic relationship, addressing them promptly transforms potential setbacks into opportunities for deeper understanding and growth. This collaborative framework allows CBT’s technical elements to achieve their maximum effectiveness.
Structured Problem-Solving and Skill Development
In CBT, you’ll learn to challenge problematic thoughts through a systematic framework that breaks complex issues into manageable components.
Your therapy sessions emphasize action-oriented learning where you practice applying problem-solving techniques to real-life situations rather than merely discussing them.
These targeted skill-building exercises equip you with practical tools to identify cognitive distortions, implement behavioral changes, and develop healthier response patterns that you can continue using long after therapy ends.
Systematic Challenge Framework
When facing persistent psychological difficulties, a systematic approach offers the most reliable path in the direction of meaningful change. The systematic evaluation process requires you to methodically address unhelpful thinking and behavior patterns through structured techniques.
This framework develops cognitive flexibility by teaching you to test assumptions rather than accepting them as facts.
- Identify specific problems by breaking complex issues into manageable components
- Generate multiple potential solutions and evaluate each option objectively
- Design behavioral experiments to test negative beliefs and gather evidence
- Establish SMART goals with clear steps for monitoring progress
Action-Oriented Learning Process
Building upon the systematic challenge framework, CBT’s action-oriented learning process transforms abstract concepts into concrete skills through structured practice.
You’ll engage in experiential learning through specific homework assignments designed to reinforce techniques introduced during sessions. These action steps move therapy beyond discussion into practical application.
Your therapist will guide you through breaking down complex problems into manageable components, establishing clear goals for each challenge you face. This structured problem-solving approach emphasizes your active participation monitoring thought patterns, practicing new responses, and gradually developing self-therapy capabilities.
Research consistently demonstrates that clients who complete between-session assignments achieve better outcomes.
Targeted Skill Acquisition
CBT’s structured approach to targeted skill acquisition forms the cornerstone of its effectiveness, teaching you specific techniques rather than merely promoting insight.
Through collaborative sessions, you’ll develop a toolkit of practical skills designed for long-term retention and application across diverse life situations.
Your therapist will guide you through learning essential abilities:
- Cognitive restructuring to identify and challenge negative thought patterns
- Behavioral activation to increase engagement in positive activities
- Problem-solving strategies to address challenges methodically
- Emotional regulation techniques to manage difficult feelings effectively
Therapeutic homework between sessions reinforces skill development through real-world practice.
This structured skill-building process typically spans 8-20 sessions, with progress measured through your increasing ability to apply these techniques independently in challenging situations.
Mindfulness Integration With Traditional CBT Approaches
As traditional Cognitive Behavioral Therapy evolved over recent decades, mindfulness practices have emerged as powerful complements to its established framework.
Mindfulness-Based Cognitive Therapy (MBCT) represents this integration, teaching you judgment-free observation of thoughts rather than challenging them directly. This approach improves cognitive integration through present moment awareness practices that foster mental flexibility.
Observe thoughts without judgment rather than challenge them, creating space for genuine mental flexibility.
Unlike traditional CBT, mindfulness techniques emphasize emotional acceptance and thought awareness without attempting immediate change. Research demonstrates these meditation benefits reduce depression relapse by 50% and improve psychological resilience through improved attention and working memory.
You’ll learn to observe your thought patterns with curiosity rather than criticism, creating distance from automatic negative thinking. This metacognitive shift allows you to relate differently to challenging emotions, breaking cycles of rumination that often maintain psychological distress.
Self-Therapy: Building Long-Term Resilience Through CBT Principles
The long-term effectiveness of Cognitive Behavioral Therapy depends largely on your ability to continue implementing its principles independently.
By developing self-reflection practices that identify personal triggers and warning signs of distress, you’ll build emotional resilience techniques that prevent symptom relapse.
Creating your personalized “emotional initial aid kit” involves several key components:
- Regular thought challenging exercises to maintain balanced thinking patterns
- Consistent practice of relaxation techniques during everyday stressors
- Journaling to track your progress and identify recurring thought patterns
- Utilization of CBT-based mobile apps for continued skill development
Adopting a growth mindset allows you to view challenges as opportunities rather than threats.
Setting meaningful personal goals while applying cognitive restructuring to daily situations transforms CBT from a temporary intervention into a sustainable lifestyle approach to mental wellness.
Frequently Asked Questions
How Does CBT Differ From Psychoanalysis and Humanistic Therapies?
Unlike psychoanalysis, CBT uses structured cognitive frameworks and practical therapeutic techniques focused on present problems rather than past experiences.
You’ll work collaboratively with your therapist, not investigate unconscious conflicts.
CBT differs from humanistic approaches through its directive, evidence-based methods that target specific thought patterns rather than promoting self-discovery.
CBT teaches measurable skills in a time-limited format, while both alternatives offer longer, less structured therapeutic expeditions with different philosophical foundations.
Can CBT Be Effective for Children and Adolescents?
Yes, CBT can be highly effective for children and adolescents when adapted to their cognitive developmental period. About 60% of youth recover after treatment, with proven benefits for anxiety, depression, OCD and PTSD.
Therapists modify techniques using developmentally appropriate language, shorter sessions, and incorporating play for younger children. The approach addresses both child development needs and unique adolescent challenges through cognitive restructuring, exposure tasks, and coping skills training.
Parent involvement often improves outcomes for younger patients.
What Is the Average Duration of CBT Treatment?
CBT typically lasts 12-16 weeks with sessions occurring once a week for about an hour.
Your treatment duration may vary depending on your specific condition anxiety might resolve in 12 weeks, while more complex issues may require longer treatment.
Session frequency is generally weekly, but this can be adjusted based on your needs.
Your therapist will regularly evaluate your progress to determine if you’ve achieved your goals or need extra sessions.
How Does Culture Influence CBT Implementation and Outcomes?
Culture greatly shapes CBT implementation and outcomes.
You’ll find that cultural sensitivity matters – when therapists recognize and respect your cultural values, treatment becomes more effective.
Research shows therapy adaptation improves outcomes, particularly when modifications address both surface elements (language, examples) and deep structures (core cultural beliefs).
While CBT works across diverse populations, its effectiveness may vary.
Therapists who develop cultural competence and incorporate your cultural context into interventions can prevent distress and improve therapeutic alliance.
Is Online or App-Based CBT as Effective as In-Person Therapy?
Research shows that online CBT demonstrates comparable effectiveness to in-person therapy for conditions like depression and anxiety.
You’ll find multiple meta-analyses confirming this equivalence, with no meaningful differences in outcomes.
App accessibility represents a significant advantage, allowing flexible scheduling and remote treatment options.
While therapist support may improve outcomes, even self-guided digital interventions produce positive results.
The evidence suggests you can confidently consider online or app-based CBT as a legitimate, effective alternative to traditional therapy formats.
If your CAR T-cell therapy fails, you have several evidence-based options. Clinicians may recommend retreatment with a second CAR T infusion (especially if you initially responded well), bispecific antibodies targeting different tumor markers, or groundbreaking combination approaches with checkpoint inhibitors. Stem cell transplantation remains a viable alternative with 59% one-year survival rates. Your next steps will depend on your specific failure pattern, tumor characteristics, and antigen expression profile. Exploring these alternatives offers renewed hope for treatment success.
Understanding CAR T-Cell Therapy Failure Patterns
When CAR T-cell therapy fails, distinct patterns emerge that help clinicians understand treatment resistance and plan subsequent interventions. Local disease progression dominates relapse patterns, with 86% of lymphoma patients experiencing recurrence at original tumor sites rather than systemic spread.
Most relapses involve both local and new lesions, while 84% of patients maintain some resolved lesions post-treatment. Certain tumor characteristics—size ≥5 cm, SUV ≥10, or extranodal origin—significantly increase failure risk and worsen survival outcomes.
Immune evasion mechanisms support these failures. CAR T cell mechanisms become compromised through antigen loss or modulation, T-cell exhaustion, and tumor microenvironment suppression may reactivate following initial treatment response, contributing to relapse. Furthermore, upregulation of immune checkpoints like PD-1/PD-L1 limits therapeutic efficacy, while treatment-induced changes in tumor architecture create further resistance pathways. Low baseline T-cell fitness from previous therapies contributes significantly to manufacturing failures and treatment inefficacy in up to 25% of cases. Following CAR T-cell failure, subsequent treatment options may include bispecific antibodies, which have shown complete responses in 14.3% of patients who experienced disease progression after initial therapy.
Evaluating Retreatment With CAR T-Cell Therapy
For patients who experience CAR T-cell therapy failure, retreatment with a second CAR T-cell infusion offers a potential salvage option with varying degrees of success. Response rates reach 89% in multiple myeloma patients who retain BCMA expression, with median progression-free survival of 8.3 months. However, efficacy depends heavily on persistent antigen expression and disease burden at relapse.
CAR T-cell retreatment provides a crucial salvage option for relapsed patients, with impressive response rates when target antigens remain expressed.
When evaluating retreatment eligibility, clinicians should consider:
- Target antigen expression (CD19 or BCMA) – retreatment is futile if the tumor has lost the target
- Response duration to initial therapy – longer initial responses generally predict better retreatment outcomes
- Patient performance status and bone marrow reserve – sufficient to tolerate potential toxicities
Manufacturing challenges remain significant, as T-cell quality may deteriorate after prior therapies, affecting the feasibility of producing effective second-generation CAR T-cells. Patients may undergo low-dose chemotherapy prior to subsequent CAR T-cell infusions to improve treatment efficacy.
Bispecific Antibodies as Alternative Immunotherapy
Bispecific antibodies represent a valuable alternative immunotherapy for patients who experience CAR T-cell therapy failure or aren’t suitable candidates for retreatment. These agents demonstrate modest efficacy with complete response rates around 14.3% post-CAR T failure, though performance is typically better in CAR T-naïve patients.
The safety profile offers distinct advantages with considerably lower rates of grade ≥3 CRS (2% vs. 8%) and neurotoxicity (<1% vs. 11%) compared to CAR T therapy. While CAR T-cells offer higher complete response rates at approximately 51% versus 36% for bispecific antibodies, this benefit must be weighed against safety considerations. Administration flexibility includes both subcutaneous and intravenous options without requiring specialized centers, caregiver supervision, or lengthy manufacturing delays. Patients may also experience less prolonged cytopenia with bispecific antibodies compared to CAR-T treatment. GPRC-directed bispecific antibodies generally show fewer infections and deaths compared to BCMA-targeted options.
Epcoritamab and glofitamab, FDA-approved for relapsed/refractory LBCL, work through dual engagement of CD19/CD3, bringing T-cells into proximity with malignant B-cells. This mechanism provides rapid access to effective therapy with manageable toxicity patterns, expanding patient eligibility beyond traditional CAR T candidates.
Novel Combination Treatment Approaches
Novel combination treatment approaches have emerged as promising strategies to address CAR T-cell therapy failures, with several groundbreaking pathways showing clinical potential. When your initial CAR-T therapy fails, these synergistic therapies may offer renewed hope by targeting multiple tumor escape mechanisms simultaneously.
- Dual-target CAR-T strategies – Tandem and bispecific CAR-T cells targeting CD19/20 or CD19/22 have achieved impressive complete response rates (71-86%) and prolonged progression-free survival in relapsed/refractory lymphomas. The CAR19/22 cocktail T-cell sequential administration demonstrated an 87.7% objective response rate and a median progression-free survival of 14.8 months in patients with relapsed or refractory B-cell non-Hodgkin lymphoma.
- Checkpoint inhibitor combinations – PD-1 blockade with pembrolizumab can reverse CAR-T exhaustion, improving response rates to 72% in solid tumors, though cytokine release syndrome risk increases. Combining these inhibitors with bispecific antibodies may enhance cancer cell recognition and improve outcomes in patients who have relapsed after CAR-T therapy.
- Epigenetic modulators – HDAC inhibitors like chidamide improve CAR-T efficacy through epigenetic remodeling and upregulation of tumor antigens, particularly when combined with BTK inhibitors. Chemotherapy can be integrated with CAR-T therapy to achieve superior curative effects by reducing tumor burden and modulating the immune microenvironment to enhance T-cell function.
Stem Cell Transplantation Options After CAR-T Failure

When CAR T-cell therapy fails to produce lasting remission, stem cell transplantation emerges as a potentially life-saving alternative pathway for patients with aggressive hematologic malignancies. Allogeneic hematopoietic cell transplantation (HCT) offers considerable hope, with 59% one-year total survival rates in LBCL patients and extending median survival to 70.2 months in B-ALL versus 10.5 months without transplant.
Various stem cell sources are utilized, with peripheral blood grafts predominating (86%). Donor matching influences outcomes considerably—matched related donors (26%) show lower non-relapse mortality, while matched unrelated (39%) and haploidentical donors (30%) remain viable alternatives. Most patients (77%) receive low-intensity conditioning regimens that prioritize immune reconstitution. Patient selection hinges on remission status, with complete remission pre-transplant correlating with better outcomes and lower relapse rates (9.5% at 24 months).
Targeting Alternative Cancer Antigens
After CAR T-cell therapy fails, oncologists must pivot to alternative antigen-targeting strategies that can overcome tumor resistance mechanisms. Immune evasion through antigen loss represents a primary failure mode, requiring exploration of different tumor markers.
Bispecific antibodies offer a promising approach by:
Bispecific antibodies bridge tumor cells to immune effectors, creating a dual-target strategy that circumvents resistance mechanisms.
- Simultaneously targeting two antigens (CD19/CD20 or BCMA/CD38), reducing escape potential
- Physically linking T-cells to cancer cells without complex engineering requirements
- Demonstrating efficacy in both hematologic malignancies and early solid tumor trials
For multiple myeloma patients, switching to BCMA-directed therapies like Abecma or Carvykti provides another avenue when CD19-targeted approaches fail. Since the effectiveness of CAR T-cell therapy depends on the lock and key mechanism between specific antigens and receptors, using alternative targets becomes crucial when primary antigens disappear. Treatment options are often tailored to individuals based on their specific cancer type and response to previous therapies. Tandem CAR constructs that feature multiple scFvs domains are increasingly being explored to prevent treatment failure by targeting heterogeneous tumor populations simultaneously. CD22-targeted constructs show promise in B-cell malignancies with CD19 loss, addressing the alternative antigens needed to counter resistant disease variants.
Clinical Trial Opportunities for Post-CAR-T Patients
For patients who’ve experienced CAR T-cell therapy failure, clinical trials investigating novel CAR constructs with improved persistence and multi-antigen targeting capabilities offer renewed hope. These next-generation approaches include constructs designed to overcome antigen escape mechanisms that frequently contribute to treatment resistance. Furthermore, antibody-drug conjugates (ADCs) in clinical trials provide targeted delivery of cytotoxic agents to cancer cells and may represent a viable alternative when conventional CAR T-cell approaches prove ineffective.
Novel CAR Constructs
Although conventional CAR T-cell therapy represents a breakthrough for many patients with relapsed or refractory hematologic malignancies, novel CAR constructs are emerging as promising alternatives for those who experience treatment failure.
Recent innovations in CAR design focus on improved specificity and reduced off-target effects, which may offer you new options when standard CAR-T approaches have failed. Logic-gated constructs represent a significant advancement, utilizing Boolean principles to create more precise targeting mechanisms. As research progresses, many of these innovations may also be applied to treat autoimmune diseases beyond cancer indications.
These advancements include:
- AND gate CAR systems requiring two antigens to be present before activation, reducing off-target toxicity
- OR gate constructs enabling recognition of multiple tumor antigens, addressing tumor heterogeneity and antigen escape
- NOT gate designs that prevent activation when encountering normal tissue antigens, improving safety profiles
These sophisticated logic-gated constructs may provide viable treatment pathways when conventional CAR-T therapy proves ineffective.
Antibody-Drug Conjugates
When CAR T-cell therapy fails to produce lasting remission, antibody-drug conjugates (ADCs) represent a promising alternative pathway with several distinct advantages. Recent innovations in antibody design have yielded remarkable therapeutic synergy, particularly with TRBC1-targeting ADCs that selectively eliminate malignant T-cells while preserving TRBC2+ normal T-cells.
Advanced targeting specificity allows ADCs to bypass CAR T persistence limitations while creating potent bystander killing effects against resistant tumor cells. Drug optimization with payloads like SG3249 has demonstrated rapid tumor clearance in preclinical models, eliminating malignancies within seven days without recurrence. Recent studies have demonstrated that ADCs can deliver cytotoxic drugs directly to tumor cells with high precision. This selective approach helps maintain immune protection while eradicating cancer cells. The development of these targeted therapies addresses the historical challenge of slow progress in T-cell lymphoma treatment compared to B-cell malignancies.
The clinical implications are significant: ADCs function independently of T-cell expansion and offer improved safety profiles by reducing fratricide risk. Early clinical trials are now advancing for relapsed T-cell malignancies, potentially transforming post-CAR-T treatment environments.
Managing Complications After Failed CAR-T Therapy
While CAR T-cell therapy can be transformative for many patients, those experiencing treatment failure must be closely monitored for persistent complications that often require specialized management. CRS management remains essential even after treatment failure, as inflammatory cascades may continue despite ineffective tumor control. Your healthcare team will implement sequential therapeutic approaches based on symptom severity.
For ongoing post-treatment care, your team will focus on:
- Extended cytokine monitoring to detect potential rebound inflammation that can emerge weeks after initial therapy
- Staged therapeutic interventions starting with tocilizumab for persistent IL-6 elevation, escalating to anakinra when needed
- Organ-specific supportive care customized to address any multi-system inflammation damage
Treatment plans are personalized according to your biomarker profile, with ferritin and CRP levels guiding pre-emptive anti-inflammatory therapy decisions. Early identification of tumor lysis syndrome is critical following failed therapy, especially in patients with high tumor burden who may develop metabolic disturbances despite treatment failure. Maintaining a strong support system during the recovery period is essential as patients navigate potential side effects and next treatment options.
Personalized Medicine Strategies After Immunotherapy Failure
Beyond managing complications, patients who don’t respond to initial CAR T-cell therapy can benefit from specifically customized alternative approaches based on their unique disease characteristics.
Your oncologist will likely recommend precision therapy options targeting the specific mechanisms of your treatment failure. If antigen loss caused your CAR T failure, next-generation dual-targeted constructs like CD22/CD19 CAR T-cells may overcome this resistance. Dual antigen CAR T approaches simultaneously target multiple tumor markers, considerably reducing the risk of cancer escape.
For patients with persistence issues, armored CAR T-cells improved with cytokine-expressing transgenes offer better durability. Alternatively, allogeneic CAR T-cell sources provide off-the-shelf options when time constraints exist. This approach follows the historical progression of personalized medicine that began with targeted therapies like imatinib for specific genetic mutations. Your personalized treatment plan will incorporate thorough molecular analysis of your tumor’s current state to select the most appropriate retargeting strategy that addresses your specific immunotherapy resistance pattern.
Emerging Cellular Therapies Beyond CAR-T
For patients who experience CAR T-cell therapy failure, medical science has developed multiple cutting-edge cellular therapy alternatives that may offer effective treatment options. These emerging therapies include allogeneic platforms like CAR-γδ cells that reduce rejection risk and iPSC-derived cellular products showing promise in diverse applications.
Three cutting-edge cellular innovations currently in clinical development:
- Regulatory T cell (Treg) therapies – Engineered to address autoimmune conditions with greater specificity than conventional immunosuppression
- Mesenchymal stem cells – Modified to deliver targeted cytokines or oncolytic viruses directly to disease sites
- CRISPR-edited allogeneic T cells – “Off-the-shelf” products that overcome manufacturing delays associated with autologous approaches
These next-generation platforms represent significant treatment alternatives when conventional CAR-T approaches fail, potentially offering reduced toxicity profiles and addressing resistance mechanisms through novel targeting strategies.
Frequently Asked Questions
How Does Insurance Coverage Work for Treatments After CAR-T Failure?
After CAR-T failure, you’ll face significant insurance challenges. Your insurance policies often require single-case agreements for subsequent treatments, causing delays. Coverage limitations are common, with insurers frequently denying follow-up therapies as “experimental” despite FDA approval. You’ll need detailed documentation to prove medical necessity. Medicare/Medicaid coverage exists under strict guidelines only. Consider engaging legal support and provider advocacy to strengthen appeals against denials for post-CAR-T treatment options.
What Psychological Support Resources Exist for Patients Facing CAR-T Failure?
After CAR-T failure, you’ll have access to improved psychological support resources. These include specialized counseling services through hospital programs and dedicated oncology social workers. You’re likely to receive structured education about managing depression and anxiety. Join support groups connecting you with others who’ve had similar experiences. Your care team will provide follow-up on psychological issues and can refer you to mental health specialists. Caregivers can access specific resources through online groups and counseling referrals.
Can CAR-T Failure Affect Eligibility for Future Experimental Treatments?
Your CAR-T failure doesn’t automatically disqualify you from experimental treatments. In fact, many clinical trials specifically include patients with prior CAR-T therapy in their eligibility criteria, particularly bispecific antibody studies. Your treatment history impact is often viewed positively, as researchers seek to understand post-CAR-T responses. However, you’ll still need to meet standard requirements for adequate organ function and performance status. Some trials are now designed with specific cohorts for patients in your situation.
How Do Post-Car-T Treatment Options Differ Between Pediatric and Adult Patients?
Post-CAR-T treatment options differ greatly between life stages. In pediatric considerations, you’ll find emphasis on sequential CAR constructs targeting different antigens (CD19→CD22) and managing frequent antigen downregulation. Adult responses typically involve lenalidomide combinations, platinum-based regimens, and antibody-drug conjugates. While children often receive dual/tri-specific CAR-T constructs for antigen heterogeneity, adults may benefit from bispecific T-cell engagers like epocoritamab. Both populations share allogeneic stem cell transplantation as a potential curative option.
What Lifestyle Modifications Might Improve Outcomes After CAR-T Failure?
After CAR-T failure, focus on moderate exercise routines customized to your energy levels—even brief walks can preserve muscle mass and reduce fatigue. Implement dietary changes emphasizing nutrient-dense foods and adequate protein to support recovery. You’ll benefit from mindfulness practices to manage treatment-related anxiety. Maintain consistent sleep patterns and stay hydrated. Track symptoms diligently to inform your care team, and consider joining support networks to address psychological impacts of relapse.
















