To qualify for Suboxone Patient Assistance Programs (PAPs), you’ll need to demonstrate a household income at or below 250% of the federal poverty level. You must submit income verification through tax returns (Form 1040) and current pay stubs for all household members. Supplementary requirements include proof of U.S. residency, an opioid dependence diagnosis from your doctor, and no public or private insurance coverage. Some programs offer $5 monthly copay options for insured patients. The specific eligibility process contains several key factors worth exploring.
Understanding Income Thresholds for Suboxone PAPs

While traversing Suboxone Patient Assistance Programs (PAPs), grasping the income thresholds is crucial for determining your eligibility. The primary qualification centers on earning at or below 250% of the federal poverty level (FPL), with no public or private insurance coverage. This threshold serves as the cornerstone for product customization options within the program. Eligible patients with insurance coverage may save with as little as $5 monthly copay contributions.
You’ll need to verify your income through appropriate documentation, such as tax returns or pay stubs. The promotional discount availability varies based on your specific income level within this threshold. The program allows for up to a 30-day supply of medication, though you must maintain proof of continued income eligibility. Private insurance patients can access copay assistance of up to $75 per month for their prescriptions. FDA approval makes these assistance programs a legitimate pathway for accessing this vital medication.
Understanding these income requirements helps secure you can access the medication assistance you need while meeting the program’s financial criteria.
Eligibility Requirements and Documentation

To qualify for Suboxone patient assistance, you’ll need to provide specific income documentation like tax returns or pay stubs if you’re uninsured, though private insurance holders don’t face this requirement.
Your doctor must submit detailed medical records confirming your opioid dependence diagnosis along with their signed authorization on the program application forms.
You must also demonstrate U.S. residency status through valid documentation, as these programs exclusively serve patients within the United States. The program is only available at participating pharmacies in the U.S.
Income Verification Methods
Qualifying for Suboxone patient assistance requires rigorous income verification through multiple documentation channels. You’ll need to submit your most recent IRS Form 1040 tax return, along with current pay stubs to validate your earnings. For dependent income calculations, you must include documentation for all household members.
If you’re self-employed, you’ll need to provide detailed financial statements and business records. Alternative employment documentation may include official employer verification letters or government assistance confirmations for programs like SNAP or SSI. Patient assistance programs can provide free medication for qualified low-income applicants. The program conducts regular cross-database checks and random audits to guarantee compliance with income requirements.
You must recertify your income annually to maintain eligibility, and any changes in your financial situation should be reported immediately to prevent disruption of benefits.
Required Medical Documentation
Securing approval for Suboxone patient assistance programs requires thorough medical documentation from both patients and healthcare providers. You’ll need to demonstrate ongoing positive clinical response through extensive documentation to meet reauthorization requirements. Your healthcare provider must maintain detailed records showing why alternatives like generic Suboxone aren’t suitable for your treatment.
| Documentation Type | Initial Application | Reauthorization |
|---|---|---|
| Clinical Response | Baseline Assessment | Ongoing Progress Notes |
| Drug Screening | Initial Test Results | Updated Screenings |
| Treatment Plan | Detailed Protocol | Plan Modifications |
| Medical Necessity | Prior Authorization | Continued Need Proof |
Your provider must submit proof of completed medication trials, adverse reactions, and treatment outcomes. Keep in mind that reauthorization depends on maintaining current clinical documentation showing therapeutic benefit and compliance with program requirements.
Residency Status Rules
While applying for Suboxone patient assistance programs, you’ll need to meet strict residency status requirements and provide detailed documentation to verify your eligibility. You must be a current U.S. resident and be prepared to submit residency documentation that proves your status.
Your income must fall within 250% of the federal poverty level, and you can’t have existing insurance coverage for Suboxone. You’ll need to submit proof through tax returns, pay stubs, or employer letters. Treatment programs are regulated under Chapter 397 of Florida law and require specific documentation for compliance. Keep in mind that income reporting exceptions may apply in certain circumstances, but you’ll need to discuss these with program providers during the review process.
The enrollment period is limited, typically covering a 30-day supply, and physician offices may restrict the number of patients they accept under these programs.
Steps to Apply for Patient Assistance
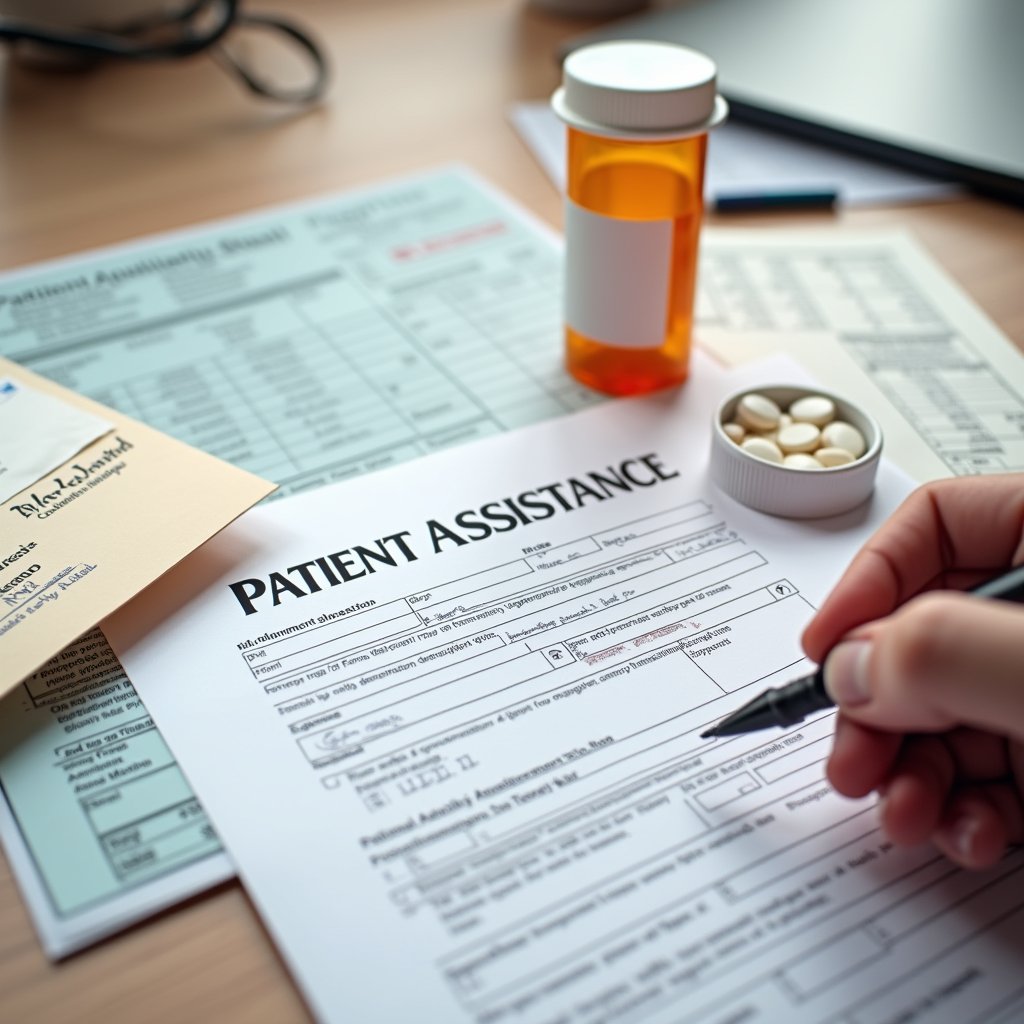
You’ll need to gather specific documentation including proof of income through tax returns or pay stubs, government-issued ID, and medical records confirming your opioid dependence diagnosis before starting the application process.
To verify your income eligibility, you must demonstrate that your annual earnings don’t exceed 250% of the federal poverty level through submission of financial documents and signed attestations.
Your completed application packet, including both physician and patient signatures, must be mailed to the Charlotte PO Box address, with processing typically occurring within standard review timelines.
Document and Proof Needs
To qualify for Suboxone patient assistance programs, you’ll need to gather several essential documents that verify your eligibility status. The patient enrollment protocols require proof of your income showing you’re at or below 250% of the Federal Poverty Level, along with verification of U.S. residency or territorial status. You must also provide documentation of your opioid dependence diagnosis and self-certify that you lack public or private insurance coverage.
Your healthcare provider needs to complete specific sections of the enrollment forms and provide a valid Suboxone prescription. You’ll need to sign an authorization allowing the program to access your health information. Annual reapplication mandates mean you should maintain copies of these documents, as you’ll typically need to resubmit them every 30 days to continue receiving assistance.
Income Eligibility Verification Process
The income eligibility verification process follows a systematic approach that starts with calculating your household’s position relative to the Federal Poverty Level.
You’ll need to provide documentation for income source status and asset assessment through multiple verification channels. Claims can be submitted and processed through the NCPDP version D.0 electronic system.
| Required Document | Verification Purpose |
|---|---|
| Recent pay stubs | Verify current earnings |
| Tax returns/W-2s | Confirm annual income |
| Bank statements | Assess financial assets |
| SS verification | Validate benefits |
| Household proof | Confirm dependents |
Your prescribing physician must complete specific application sections while you submit proof of residency and opioid dependence diagnosis. The program administrators will review your documentation to guarantee you’re within the 250% FPL threshold and don’t have existing prescription coverage. You’ll need to recertify annually by submitting updated financial records.
Application Submission Timeline
Submitting a Suboxone patient assistance application involves several time-sensitive steps that must be completed in the correct sequence.
You’ll need to start by gathering your current proof of income, valid insurance cards, and Suboxone prescription documentation. Next, you’ll complete the patient section of the application and obtain your healthcare provider’s signature on the required forms. Your provider must verify your eligibility and complete their designated sections.
Once you’ve assembled all materials, including signed authorization forms, you’ll mail the complete package to the program’s administrative office. Only qualified practitioners with proper certification can prescribe and verify your Suboxone prescription paperwork.
Processing times vary by program, and you may receive requests for supplementary documentation during the program approval process. If your application is incomplete or missing signatures, you’ll need to resubmit with all required materials, which can delay your assistance.
Key Program Limitations and Restrictions
While Suboxone patient assistance programs offer valuable support for opioid dependence treatment, strict eligibility criteria and operational constraints govern participation. You’ll need to navigate several medication access limitations and understand cost reduction strategies to successfully participate in the program.
| Requirement Type | Key Restriction |
|---|---|
| Income Level | ≤250% Federal Poverty Level |
| Insurance Status | No public/private coverage |
| Program Duration | 12-month maximum term |
| Physician Limits | 3 patients per doctor |
You must meet specific minimum age requirements (16+ years) and maintain US residency throughout participation. The program won’t allow extensions beyond the initial one-year period, and you’ll receive medication in 30-day supply increments. Remember, you can’t combine this assistance with other insurance benefits or copay programs.
Available PAP Options and Resources
You’ll need to meet strict eligibility requirements, including falling below 250% of the federal poverty level and having no existing insurance coverage, to qualify for Suboxone patient assistance programs.
Your options include manufacturer programs like Here to Help PAP which provides 30-day supplies through pharmacy cards, and INSUPPORT Copay Assistance which can reduce costs to $5 for privately insured patients.
Moreover, you may find state-specific opportunities through federal grants and regional programs that adjust income thresholds based on your location and family size.
Major Program Eligibility Rules
To qualify for Suboxone patient assistance programs, you’ll need to meet specific eligibility requirements that vary between the two main options: INSUPPORT Copay Assistance and Suboxone Here to Help. Understanding these key program distinctions is essential for securing uninsured patient coverage and meeting product quality requirements.
Key eligibility rules include:
- You must have a confirmed opioid dependence diagnosis from your healthcare provider
- INSUPPORT requires active private insurance coverage, while excluding government programs like Medicare or Medicaid
- Suboxone Here to Help serves uninsured patients with incomes at or below 250% of the Federal Poverty Level
- You’ll need to be at least 16 years old for Suboxone Here to Help, and your physician can’t exceed enrolling three patients
Documentation requirements include income verification and healthcare provider authorization forms for processing your application.
Accessing Financial Support Resources
Several financial support options exist for patients seeking Suboxone treatment assistance. If you’re uninsured, you can access pharmacy discount programs and manufacturer support through Suboxone’s website to reduce medication costs. These uninsured patient resources often provide significant savings at retail pharmacies.
For affordability considerations, you’ll find multiple funding streams to investigate. You can use FSA or HSA accounts to pay for treatment with pre-tax dollars, while INSUPPORT® offers copay assistance if you have insurance coverage. State and federal grants may provide additional funding options.
You’ll also find support through public health services and ongoing care coordination programs. Your local pharmacy partnerships can help facilitate medication access and explain available discount options for your specific situation.
State-Specific PAP Opportunities
State-specific Patient Assistance Programs (PAPs) maintain distinct eligibility requirements and coverage options across different regions. You’ll find that managed care policies vary considerably between states, particularly regarding Medicaid expansion and coverage for Suboxone treatment. Your out-of-pocket costs may differ based on your location and program availability.
Your state’s Medicaid expansion status directly impacts your eligibility for additional assistance programs and coverage options. You must verify your state’s specific PAP requirements, as income thresholds and documentation needs can vary by region. Each state maintains different physician participation limits and prescription duration restrictions. Your local program may offer complementary resources alongside federal assistance, including manufacturer savings cards and copay reduction options.
When traversing state-specific opportunities, you’ll need to research your region’s particular guidelines while meeting basic residency and income verification requirements.
Income Verification Process
The income verification process for Suboxone patient assistance follows strict federal guidelines requiring applicants to demonstrate household earnings at or below 250% of the Federal Poverty Level (FPL).
When maneuvering healthcare bureaucracy, you’ll need to submit specific documentation for determining program credibility:
| Document Type | Timeframe Required | Status |
|---|---|---|
| Pay Stubs | Last 3 months | Primary proof |
| Bank Statements | Last 3 months | Supporting document |
| Tax Returns | Most recent year | Alternative proof |
You must guarantee all documentation reflects your current financial situation within the past 12 months. Your healthcare provider will validate your application by confirming medical necessity and submitting required forms through approved channels, whether by mail, fax, or online portals.
Duration and Renewal Guidelines
While traversing Suboxone assistance programs, you’ll need to understand specific duration limits and renewal protocols that govern prescription coverage. The standard prior approval process includes strict medication volume limits and renewal frequency requirements that you must follow.
Key program guidelines include:
- You’ll receive up to 12 months of coverage for combination products, with your initial month allowing 2 prescription fills
- You’ll need to submit treatment plans documenting medical necessity for renewals
- You’re limited to a maximum daily dose of 24mg buprenorphine, regardless of form
- You’ll get special considerations if pregnant (9-month initial approval) or breastfeeding (2-month postpartum renewals)
Your physician must verify compliance through the Controlled Substances Database before authorizing prescription renewals, ensuring you’re not concurrently using opioids or benzodiazepines.
State-Specific Program Variations
Pronounced variations exist across state-specific Suboxone assistance programs, with each jurisdiction maintaining distinct eligibility criteria, funding mechanisms, and coverage parameters.
You’ll find that 31% of states directly subsidize buprenorphine treatment, while eight states specifically allocate federal block grants for this purpose.
Through prescription assistance collaborations, you’re more likely to access coverage in states with expanded Medicaid programs and targeted funding streams. Treatment program subsidies differ remarkably, with private nonprofits offering greater access than public facilities. The Substance Abuse Prevention and Treatment Block Grant provides funding for up to 55% of treatment services.
If you’re in a state with technical assistance programs, you’ll benefit from 1.18x higher odds of accessing buprenorphine services. State Prescription Assistance Programs (SPAPs) in six states provide extra coverage options, though eligibility requirements differ by location. Prior authorization requirements may affect your access in certain states.
Physician Participation Requirements
Building upon state-specific variations, physicians must fulfill strict administrative and licensing requirements to participate in Suboxone assistance programs. The program notification process requires detailed documentation and ongoing recordkeeping requirements to maintain compliance.
- You’ll need current DEA Schedule III registration and completion of the mandatory 8-hour OUD training or addiction medicine board certification for prescribing privileges. Removing the X-waiver requirement has significantly reduced barriers for physicians to provide treatment.
- You must manage patient enrollment caps, typically limited to 3 patients simultaneously per physician, while tracking program durations
- You’re responsible for verifying patient eligibility, including insurance status and income documentation, plus submitting necessary paperwork to program administrators
- You’ll maintain thorough records for audits, including treatment plans, authorization letters, and recertification documentation, while adhering to program-specific protocols for continued participation
Alternative Financial Support Methods
Several alternative financial support methods exist for patients seeking affordable Suboxone treatment beyond traditional assistance programs. Understanding patient copay contributions leads to multiple options: you can utilize copay assistance cards that reduce monthly costs to as low as $5 if you have private insurance, or access sliding fee scale clinics that adjust treatment costs based on your income level.
Supplemental financial assistance programs include state and federal grants for addiction treatment, particularly if you’re uninsured. You’ll need to provide income documentation to qualify. Non-profit organizations offer financial counseling and connect you to regional resources.
If you have employer-sponsored insurance, you can use FSA/HSA accounts to cover prescription costs with pre-tax dollars, though annual contribution limits apply. Each option requires specific eligibility criteria and may have coverage caps.
Frequently Asked Questions
Can Family Members Share a Single PAP Card for Suboxone Treatment?
You can’t share PAP cards among family members for Suboxone treatment. Each card is strictly tied to one individual patient and requires personal income verification during the application process. You’ll need to submit your own application with unique documentation if you’re seeking assistance.
The programs are designed for individual use only, and sharing cards violates program rules and could result in termination of benefits.
What Happens if Income Changes During the Program Participation Period?
If your income changes during program participation, you’ll generally maintain your current benefits until the enrollment period ends, as most PAPs don’t require mid-term income verification. However, you should review your program’s specific income eligibility requirements and program discontinuation criteria.
While it’s recommended to report significant income changes, it typically won’t affect your active enrollment. For future applications, you’ll need to meet the income thresholds in place at that time.
Are Homeless Individuals Eligible for Suboxone Patient Assistance Programs?
Yes, you can access Suboxone patient assistance programs while homeless, though you’ll need to meet certain requirements. Programs often work with local support services to verify your status and treatment readiness.
You’ll typically undergo mental health screening and demonstrate ability to follow treatment protocols. Many programs now accept temporary housing options as sufficient proof of stability. Contact community health centers or mobile health units to connect with available assistance programs.
Can Multiple Doctors Prescribe Suboxone Under the Same PAP Application?
No, you can’t have multiple doctors prescribe Suboxone under the same PAP application. The program strictly prohibits simultaneous prescriptions and multi provider participation.
You’ll need to work with a single designated prescriber who’ll manage your treatment throughout the program period. Your prescriber must maintain enrollment records and coordinate your care directly. This rule helps guarantee medication safety and proper treatment monitoring under the program’s guidelines.
Do Pharmacies Charge Additional Fees When Using PAP Benefits?
While Patient Assistance Programs (PAPs) typically cover medication costs, you’ll need to check with specific pharmacies about their payment processing fees and dispensing policies.
The background materials don’t explicitly state whether pharmacies can charge supplementary fees when using PAP benefits. It’s recommended that you contact both your chosen pharmacy and the PAP administrator directly to verify any potential charges before filling your prescription.