Current hospital nitrous oxide regulations require you to move from central piped systems to portable delivery units, reducing gas leakage by up to 99%. You’ll need real-time monitoring systems, dual alarm protocols, and documented exposure tracking for both patients and staff. Your facility must implement waste shepherds, pin-index verification, and WAGD systems while adhering to stricter dispensing controls. Understanding these complex regulatory changes will guarantee your facility’s continued compliance and operational efficiency.
Major Regulatory Shifts in Medical Nitrous Oxide Use

While medical nitrous oxide remains an essential analgesic and sedative agent, significant regulatory changes in the year 2025 have transformed its administration protocols across healthcare settings. You’ll find stricter oversight of self-administered alternatives, with the FDA issuing thorough safety alerts against recreational use and implementing tighter controls on all canister sizes. The regulation aims to prevent substance abuse deaths associated with recreational misuse.
Industry association guidelines now mandate behind-the-counter status for medical applications, requiring detailed documentation and professional dispensing. Healthcare facilities must implement proper WAGD systems to ensure staff exposure is minimized during administration. In Pennsylvania, new regulations allow dental hygienists to monitor nitrous oxide under dentist supervision. You’re required to comply with augmented monitoring protocols, particularly in dental settings where strict supervision requirements apply.
The American Society of Anesthesiologists recommends deactivating central piped systems in favor of portable supply units, reflecting a broader shift toward more controlled delivery methods. These changes aim to minimize risks while maintaining nitrous oxide’s therapeutic benefits under proper medical supervision.
Environmental Impact and Emission Control Measures

The systematic phase-out of central nitrous oxide systems in major hospitals has yielded up to 99% reductions in gas leakage, while portable tank implementation requires strict protocols for storage, tracking, and disposal to maintain these environmental gains. Four major hospitals have completely eliminated their central nitrous oxide systems.
You’ll find that proper tank management demands real-time monitoring systems to track discrepancies between purchased quantities and clinical usage, enabling rapid identification of potential leaks or inefficiencies. With nitrous oxide lasting 114 years in atmosphere, healthcare facilities must prioritize preventing even minor leaks from their delivery systems. Hospitals are implementing waste shepherds in each unit to ensure proper gas handling and disposal protocols are followed.
Healthcare facilities targeting 50% emission reductions must combine these infrastructure changes with clinical practice shifts in the direction of regional and intravenous anesthetic alternatives, as recommended by the American Society of Anesthesiologists.
Central System Phase-Out Benefits
Significant environmental and operational benefits emerge from phasing out centralized nitrous oxide systems, as demonstrated by NYC Health + Hospitals’ achievement of over 50% reduction in annual anesthesia emissions. You’ll find that central systems leak 85-99% of purchased gas before clinical use, making their removal vital for environmental protection and operational workflow impacts. N2O’s 273 times warming potential compared to CO2 makes its reduction crucial for climate action. Portable cylinder delivery has proven to be a more efficient and environmentally responsible alternative for essential clinical uses like labor pain management. With 40% of Quebec facilities already eliminating centralized systems, there is clear momentum toward sustainable healthcare practices.
Key benefits of central system phase-out include:
- Carbon footprint reduction of up to 2,000 metric tons per facility, as seen at Bellevue Hospital
- Improved care quality through shift to regional or IV anesthesia alternatives
- Elimination of occupational exposure risks from system leaks, improving staff safety
- Cost savings from reduced maintenance, leak detection, and gas purchasing requirements
These improvements align with ASA recommendations and support hospitals’ 2030 carbon reduction targets while maintaining clinical excellence.
Tank Management Best Practices
Building on the environmental gains from central system removal, proper tank management protocols now serve as primary safeguards against nitrous oxide emissions in healthcare facilities. You’ll need to implement strict cylinder rotation practices and maintain detailed inventory management logs to prevent gas expiration and minimize waste generation. Due to new FDA safety advisories, facilities must document all nitrous oxide inventory movements with heightened scrutiny. Automatic sprinklers must be installed in all medical gas storage rooms per current requirements.
Your facility must establish closed-loop delivery systems and conduct regular pressure testing to detect potential leaks. Install check valves and alarms on manifolds exceeding 2,000 ft³ to prevent dangerous backflow scenarios. Guarantee you’re storing tanks in properly vented enclosures when capacity is below 2,000 ft³, and maintain strict segregation of at least 20 feet between flammable and non-flammable gases. You must also regularly inspect valves and connections using approved detection methods to prevent environmental releases. Since nitrous oxide is a non-flammable medical gas, it can be safely stored with other medical gases like carbon dioxide, medical air, and helium in the same storage room.
Greenhouse Gas Reduction Goals
Under stringent environmental regulations, healthcare facilities must now achieve a 75% reduction in nitrous oxide emissions by 2025 through thorough control measures. Comprehensive data analysis reveals that moving from traditional pipe systems to cylinder-based delivery methods can greatly decrease atmospheric waste. Facilities must maintain suitable construction standards to ensure proper medical gas compliance and safety.
Current regulatory trends emphasize strict emission controls and detailed monitoring protocols.
- You’ll need to implement real-time tracking systems to monitor gas usage patterns and identify potential leaks or inefficiencies
- You must replace outdated in-wall pipe systems with monitored cylinder carts, reducing emissions by up to 99%
- You’re required to establish rigorous inventory controls to prevent unauthorized use and track consumption metrics
- You should integrate environmental impact assessments into your facility’s sustainability reporting, documenting emission reduction progress against established benchmarks
Portable Systems vs. Central Piped Distribution
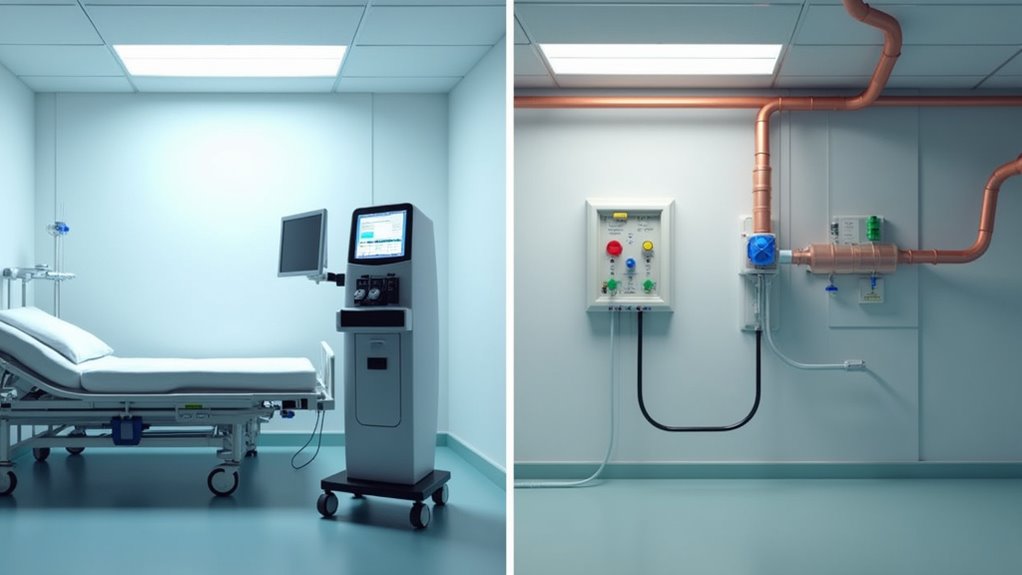
Three critical factors differentiate portable nitrous oxide systems from central piped distribution in modern healthcare facilities. Initial, portable systems demonstrate a dramatic 99% reduction in gas loss compared to central systems’ 70-90% leak rates, enabling scalable implementation plans across diverse clinical settings.
Second, you’ll find portable cylinders offer flexible deployment models that allow precise control in non-OR environments while eliminating infrastructure-related waste. Third, you’re achieving significant cost savings through reduced maintenance requirements and eliminated leak-related expenses.
When you’re moving to portable systems, you’ll need to integrate cylinders with existing anesthesia carts and implement extensive staff training protocols. This switch aligns with ASA’s current recommendations and supports your facility’s emission reduction targets while maintaining clinical flexibility in nitrous oxide administration.
Safety Protocols and Clinical Guidelines Update
Modern N2O monitoring requirements mandate real-time oxygen analysis with dual alarm systems and continuous airway patency verification during clinical administration.
You’ll need to implement improved scavenging protocols with efficiency testing to meet stringent emission control standards while maintaining workplace safety parameters. The shift away from central pipe systems has significantly reduced gas waste and environmental impact.
Your facility’s shift to portable N2O delivery systems requires supplementary safety measures, including pin-index verification systems and documented exposure tracking for both patients and personnel.
Monitoring Requirements Evolution
Safety protocols and clinical guidelines for nitrous oxide monitoring have undergone significant evolution, driven by heightened risk awareness and technological advances in delivery systems. You’ll need to implement extensive staff exposure monitoring and effective risk mitigation strategies that align with updated NIOSH recommendations.
Key monitoring requirements now include:
- Continuous tracking of exposure levels against the 25 ppm threshold using advanced detection systems
- Documentation of patient-specific data with precise timestamps in digital monitoring logs
- Regular verification of 12+ safety features, including audio/visual alerts in delivery systems
- Annual competency assessments ensuring proper ventilation practices and emergency response protocols
Since OSHA requirements are surprisingly absent in the medical field, implementing voluntary compliance measures is crucial for workplace safety. To maintain compliance, you must integrate these improved monitoring standards while maintaining proper documentation of BLS certifications and clinical competency affidavits. Your facility’s monitoring program should emphasize both occupational safety and patient care standards. The requirement of 1000 hours clinical experience serves as a critical prerequisite for personnel authorized to monitor nitrous oxide administration in healthcare settings.
Portable System Safety Standards
Building upon established monitoring protocols, portable nitrous oxide delivery systems now require heightened technical specifications and rigorous operational standards in 2025. You’ll need to implement portable system upgrades that align with regulatory impact evaluations focused on patient and provider safety.
| Component | Safety Requirement |
|---|---|
| Demand Valves | Active flow control with dual redundancy |
| Scavenging System | NIOSH-compliant 25 ppm exposure limit |
| Alert Mechanisms | Audio-visual warnings for system failures |
| Ventilation Controls | Minimum 12 air changes per hour |
| Maintenance Protocol | Quarterly calibration verification |
The updated standards mandate integrated safety features with fail-safe mechanisms, automated shutdown protocols, and real-time exposure monitoring. You must guarantee your portable units comply with bolstered scavenging requirements and maintain documented regulatory compliance through systematic performance verification and risk assessment procedures.
Training Requirements for Healthcare Providers
Three foundational pillars support the 2025 healthcare provider training requirements for nitrous oxide administration: structured educational programs, clinical competency validation, and state-specific compliance measures.
Healthcare providers administering nitrous oxide must master three core elements: education, competency validation, and state compliance standards by 2025.
You’ll need to complete a thorough four-part training sequence that incorporates:
- Pre-course preparation, including required pharmacology readings and case analyses
- Video-based modules covering pain management and legal frameworks
- Hands-on clinical training with at least three supervised patient cases for competency validation
- State-mandated coursework meeting regional requirements like Minnesota’s 12-hour minimum
Your competency validation now requires instructor feedback protocols during equipment operation, patient monitoring, and emergency response scenarios. You must demonstrate proficiency in fail-safe device operation and positive pressure respiration techniques while adhering to strict environmental safety protocols and pediatric-specific administration guidelines.
Cost Implications and Economic Considerations
You’ll uncover substantial return on investment when migrating to portable nitrous oxide systems, with facilities reporting up to 99% reduction in gas leakage compared to traditional piped infrastructure. Your initial costs for retrofitting anesthesia carts with cylinder attachments will be offset by dramatic reductions in supply chain expenses and waste-related losses, as traditional piped systems typically lose 70-90% of gas through facility infrastructure.
Your procurement costs will further decrease through optimized bulk purchasing of cylinders, while simultaneously reducing your facility’s exposure to environmental compliance risks and potential regulatory penalties.
Portable System Investment Returns
Healthcare facilities routinely achieve substantial returns on portable nitrous oxide system investments through multifaceted cost reductions. You’ll find significant anesthesia cost savings through the elimination of piped infrastructure maintenance and reduced gas waste, while maintaining high patient convenience outcomes.
Your facility can reduce gas consumption by 70-90% compared to traditional systems, as demonstrated by Providence’s 99% reduction in nitrous oxide loss after converting to portable cylinders.
You’ll eliminate recurring maintenance costs associated with fixed gas delivery infrastructure.
Your operational costs decrease through precise delivery systems that minimize anesthesia cart waste.
You can expand service offerings to non-traditional settings without capital-intensive piping installations.
These returns directly support budget optimization while meeting Joint Commission recommendations for modern gas delivery systems.
Supply Chain Cost Benefits
While moving to portable nitrous oxide systems requires initial investment, the supply chain cost benefits deliver substantial financial advantages across multiple operational domains. You’ll achieve operating margin improvement through simplified inventory tracking, optimized cylinder sourcing, and elimination of bulk purchasing requirements. The shift enables precise asset utilization optimization by allowing your facility to order smaller quantities based on actual usage patterns.
Your supply chain costs decrease greatly when you eliminate pipeline infrastructure maintenance, reduce technical labor requirements, and streamline distribution logistics. The portable systems’ targeted ordering capabilities help you negotiate better pricing with suppliers while minimizing storage expenses. You’ll also benefit from reduced energy consumption in storage facilities and lower transportation costs, as cylinder delivery replaces complex pipeline network maintenance requirements.
Supply Chain Management and Storage Updates
Managing nitrous oxide storage in medical facilities demands rigorous adherence to updated 2025 fire safety protocols and storage specifications. You’ll need to implement thorough building security protocols and emergency response procedures while maintaining strict separation requirements between oxidizing gases and combustible materials.
- You must guarantee storage rooms feature 1-hour fire-rated walls with ¾-hour fire-rated doors, plus ventilation intakes 6 inches from the floor and exhausts near the ceiling
- You’re required to maintain 20-foot separation between oxidizers and flammables, reducible to 5 feet with automatic sprinklers
- You can’t store medical air compressors or vacuum pumps in central supply areas
- You’ll need to secure emergency power connections for all central supply systems, guaranteeing continuous operation during outages
Patient Care Adaptations and Best Practices
Modern patient care protocols for nitrous oxide administration require thorough adaptations to meet 2025 safety standards. You’ll need to implement real-time gas monitoring systems and enforce strict exposure limits of 100 ppm over 8-hour periods. When utilizing patient administered protocols with 50/50 nitrous oxide/oxygen mixtures, you must maintain constant staff supervision and documentation.
Your facility should move from central piped systems to portable delivery units, while exploring alternative anesthesia modalities in high-exposure areas. You’re required to restrict nitrous oxide use to level I anesthesia in office settings, allowing patient ambulation. Guarantee your staff completes mandatory COSHH assessments and maintains proper ventilation controls. You must also establish clear emergency protocols for leak detection and immediate evacuation procedures.
Compliance Standards for New Hospital Construction
As healthcare facilities move away from centralized nitrous oxide infrastructure, new hospital construction must incorporate stringent compliance standards for portable gas delivery systems. You’ll need to implement facility renovation requirements that align with COSHH exposure limits and ASA 2024 guidelines while optimizing operational workflow for N₂O management.
- Install real-time gas monitoring systems with automated alerts when levels approach the 100 ppm TWA threshold
- Design dedicated storage areas for portable N₂O cylinders with proper ventilation and security controls
- Integrate automated inventory tracking systems for cylinder management within the facility’s digital infrastructure
- Configure specialized HVAC systems in ORs and labor/delivery areas to maintain negative pressure and guarantee proper gas evacuation
These technical requirements must undergo regular audits to verify compliance with evolving international standards and Joint Commission accreditation criteria.
Cross-Departmental Implementation Strategies
While moving to portable N₂O systems requires complex organizational coordination, you’ll need to execute a multi-phased implementation strategy across clinical departments to minimize operational risks. Interdepartmental coordination through dedicated oversight committees guarantees standardized equipment maintenance protocols across OR, dental, and labor/delivery units.
| Department | Critical Requirements |
|---|---|
| Clinical | Real-time gas monitoring, leak detection |
| Supply Chain | Cylinder tracking, demand forecasting |
| Facilities | Storage optimization, safety protocols |
| Environmental | Emissions benchmarking, compliance reporting |
You’ll need to establish cross-functional training modules and conduct regular mock drills for cylinder replacement procedures. Partner with medical gas vendors to optimize delivery schedules and implement cylinder-tracking systems. Your facility’s success depends on maintaining clear communication channels between environmental, clinical, and purchasing teams while standardizing troubleshooting procedures across all departments using N₂O.
Frequently Asked Questions
How Long Does It Take Hospitals to Complete the Transition Process?
You’ll need 12-18 months to complete a full N2O system conversion, depending on your facility’s size and complexity. Critical path activities include inventory planning, equipment maintenance protocols, and phased implementation across departments.
The most time-intensive phases are infrastructure modifications and staff training. You must maintain uninterrupted patient care throughout the changeover, which requires careful scheduling and redundant systems during the transition period.
What Happens to Existing Central Piped Systems During Emergency Power Outages?
During emergency power outages, your centralized N2O systems automatically initiate protective shutdown protocols, even if you’ve got redundant power supply systems in place. You’ll see immediate valve closures triggered by your centralized monitoring systems to prevent uncontrolled gas releases.
You must maintain portable cylinder backups as a critical failsafe, since they’ll become your primary delivery method. You’re required to follow updated emergency response protocols to minimize leak risks during these events.
Can Patients Request Specific Nitrous Oxide Delivery Methods for Their Procedures?
You can request specific nitrous oxide delivery methods, but your choice must align with strict clinical protocols and safety requirements. Your hospital’s patient education requirements mandate that you receive detailed briefing on risks and limitations.
While flexible delivery options exist, facility-specific portable system maintenance schedules and continuous monitoring protocols may restrict certain methods. Your care team must evaluate your medical history and obtain documented consent before accommodating delivery preferences.
How Do Rural Hospitals Manage Portable Tank Logistics in Remote Locations?
You’ll need to implement rigorous portable tank storage requirements in your rural facility, including temperature-controlled environments and secured access points. Your team must conduct periodic nitrous oxide tank inspections to verify integrity and compliance.
You’ll want to maintain larger reserve inventories to offset delivery challenges, while utilizing remote monitoring systems to track usage patterns. Partner with specialized logistics carriers who can navigate difficult terrain for consistent resupply operations.
Are There Backup Options if Portable Systems Malfunction During Critical Procedures?
You’ll need multiple backup options ready if your portable N₂O systems fail during procedures. Guarantee you’ve installed backup power sources for monitoring equipment and maintain strict routine maintenance schedules.
You must cross-train your staff on rapid deployment of alternative methods like regional anesthesia or IV sedation. Keep emergency reserve cylinders on standby, and maintain redundant supply chains with multiple gas vendors to prevent critical shortages.