Nighttime anxiety often intensifies when sleep deprivation disrupts normal brain regulation. As you lie awake, the amygdala becomes hyperreactive while activity in the prefrontal cortex drops, reducing your ability to manage emotional responses. Sleep loss can trigger more than a 60% increase in anticipatory brain activity, amplifying anxious thoughts and sensations. This creates a self-reinforcing cycle: anxiety delays sleep onset, and prolonged wakefulness fuels worry through rumination and clock-watching. Consistently sleeping fewer than five hours a night raises anxiety risk by about 40%, while getting seven or more hours can reduce it by 63%. Understanding these neurological mechanisms helps clarify how this cycle forms and how it can be interrupted.
The Brain’s Role in Nighttime Anxiety and Sleep Loss
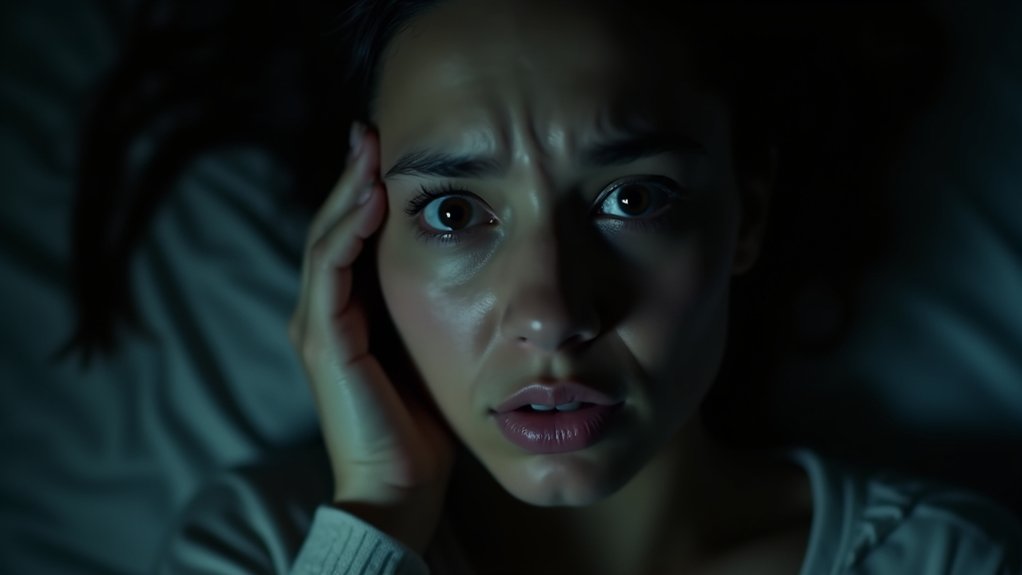
When you lose sleep, your brain doesn’t simply function with less efficiency, it undergoes measurable neurological changes that actively amplify anxiety. Your amygdala becomes hyperreactive, triggering exaggerated emotional responses to both threatening and benign stimuli. Simultaneously, your prefrontal cortex, the region responsible for emotional regulation, shows decreased activity and weakened connectivity with the amygdala. This disconnect leaves you vulnerable to unchecked emotional reactivity.
Your insula, which processes emotional sensitivity, becomes increasingly activated during sleep deprivation, amplifying anxiety perception. Enhanced beta wave activity in your frontal regions reflects heightened hypervigilance and rumination. Sleep deprivation also disrupts the neurochemical balance that supports emotional stability, with substantial noradrenaline reduction typically occurring during restorative REM sleep now prevented.
These neurological shifts aren’t subtle: one sleepless night elevates anxiety by approximately 30%. REM sleep typically restores prefrontal control over limbic structures, but deprivation disrupts this indispensable recalibration, perpetuating the anxiety cycle. Research shows that sleep deprivation triggers over 60% increase in anticipatory emotional brain activity, particularly in naturally anxious individuals.
This hyperactivity in emotion-processing regions mirrors the brain patterns observed in individuals diagnosed with anxiety disorders, suggesting that chronic sleep loss could sensitize individuals to greater anxiety levels. The convergence of these neurological changes creates a biological foundation for the development of persistent anxiety when sleep deprivation becomes chronic. As a result, understanding the link between sleep deprivation and anxiety is crucial for developing effective interventions. Incorporating strategies to improve sleep may enhance the effectiveness of individual therapy for anxiety, thereby addressing both the symptoms and underlying causes.
How Anxiety and Insomnia Create a Vicious Cycle
The relationship between anxiety and insomnia isn’t unidirectional, it’s bidirectional and self-perpetuating. You experience anxiety at night, which prevents sleep onset, then sleep deprivation intensifies anxiety symptoms the following evening. This cycle compounds over time, creating escalating mental health consequences.
| Direction | Mechanism | Outcome |
|---|---|---|
| Insomnia → Anxiety | Sleep deprivation heightens brain hyperarousal | Anxiety disorders develop within 10 years |
| Anxiety → Insomnia | Racing thoughts prevent sleep initiation | Chronic wakefulness amplifies worry |
| Mutual Reinforcement | Clock-checking and rumination intensify both | Detrimental cycle strengthens |
Nearly three-quarters of anxiety disorder participants report sleep disturbances, while 24-36% experience clinical insomnia. Early detection of insomnia aids mental disorder identification. These neurological changes involve alterations in the hypothalamic-pituitary-adrenal network that disrupt normal sleep regulation mechanisms.
Research examining data from over 25,000 adults demonstrated that chronic insomnia significantly increased the risk of developing anxiety disorders even when accounting for age, gender, and educational factors. Untreated sleep and anxiety issues have compounding impacts on overall health outcomes. Without intervention, you’ll experience compounded effects: higher healthcare costs, reduced productivity, and deteriorating emotional regulation.
What the Research Shows About Sleep Duration and Anxiety Risk

You’ll want to understand that research consistently identifies 7, 9 hours as the ideal sleep window, with your anxiety risk rising sharply when you fall below this threshold, particularly if you’re sleeping fewer than 5 hours nightly.
Studies show gender differences in vulnerability, with males experiencing stronger associations between short sleep and anxiety symptoms than females, though both sexes face increased risk at critically reduced durations. This dose-response pattern means your anxiety doesn’t simply spike at one point; rather, each hour of sleep loss below the 7-hour floor incrementally elevates your likelihood of experiencing clinically significant anxiety symptoms.
Women appear particularly vulnerable to anxiety when sleeping ≤6 hours or ≥9 hours, suggesting a narrower optimal sleep window for this population. A longitudinal study of first-year medical students found that inadequate sleep significantly increased the odds of mild, moderate, and severe anxiety compared to adequate sleep durations. Research indicates that approximately 34% of the US population is affected by anxiety disorders, underscoring the widespread public health significance of understanding sleep’s protective role.
The 7-Hour Threshold
Research consistently identifies seven hours as a critical sleep duration for anxiety management. When you sleep fewer than seven hours, you’re considerably more likely to experience anxiety before bed and nighttime worry that keeps you awake. Studies show that sleeping seven or more hours reduces your anxiety odds by 63% compared to shorter sleep durations. Why do I get anxious at night? Partly because insufficient sleep dysregulates your nervous system.
Very short sleep, under five hours, increases anxiety risk by 40%, while sleep between five and seven hours elevates it by 17%. Conversely, achieving seven to nine hours of nightly sleep establishes your brain’s ideal baseline for emotional regulation and reduces future anxiety symptoms substantially.
The impact extends beyond anxiety alone, as inadequate sleep and mental distress are closely interconnected, with research demonstrating that those sleeping six hours or less experience nearly triple the odds of frequent mental distress. Sex differences in sleep vulnerability mean that women may experience anxiety more acutely than men in response to short sleep duration, particularly when combined with evening chronotypes that misalign with social schedules. During periods of high stress such as pandemics, residents’ sleep should receive attention to prevent anxiety from worsening and to support overall mental well-being.
Gender Differences in Risk
While nighttime anxiety and sleep disruption affect both men and women, research reveals a striking gender disparity: women experience markedly higher rates of poor sleep quality and anxiety-related sleep problems. Studies show 65.1% of women report poor sleep compared to 49.8% of men, with anxiety at bedtime cited by 51% of women versus 42% of men as a primary culprit. Women also report greater pre-sleep arousal, both cognitive and somatic, a key factor perpetuating insomnia.
Additionally, 33% of women wake nightly compared to 27% of men. These gender differences in nighttime anxiety emerge prominently during early-to-mid adulthood, often intensifying after puberty. Hormonal fluctuations across reproductive stages further modulate sleep architecture and anxiety vulnerability in women, suggesting both biological and psychological mechanisms underlie these disparities.
Importantly, the gender difference in poor sleep quality persists even after adjusting for depression and socioeconomic factors, indicating that biological factors play a significant independent role. In adolescent populations, girls demonstrate significantly higher insomnia severity scores and experience greater wake after sleep onset compared to boys, revealing that gender-based sleep disparities begin early in development. Women with children face compounded sleep challenges, as caregiving responsibilities create additional nighttime disruptions and worry that intensify their anxiety-related sleep problems.
Dose-Response Anxiety Pattern
The relationship between sleep duration and anxiety doesn’t follow a simple linear trajectory, instead, it traces a U- or J-shaped curve where both inadequate and excessive sleep associate with heightened anxiety risk. Research consistently demonstrates that sleeping less than 7 hours or more than 8 hours correlates with markedly higher anxiety odds compared to the 7, 8 hour sweet spot.
Adults sleeping under 7 hours experience approximately 5.86-fold greater anxiety risk, while those exceeding 8 hours face roughly 1.88-fold increased odds. This nonlinear dose-response pattern explains why you might experience night anxiety or anxiety when sleeping irregularly. Sleep quality compounds this relationship: poor sleepers show 3.85-fold higher anxiety odds.
The data suggests anxiety every night intensifies at sleep extremes, making consistent 7, 8 hour routines protective. This J-shaped association is particularly pronounced in males, where long sleep duration exceeding 8 hours correlates with 76% higher odds of anxiety symptoms compared to the recommended sleep window.
Why Nighttime Amplifies Worry and Racing Thoughts

When external distractions fade at night, you’re left alone with your thoughts, a shift that activates your brain’s default mode network and intensifies ruminative cycles. You may notice that your bed becomes a conditioned cue for anxiety itself, especially after repeated nights of racing thoughts in that environment. Additionally, you’re likely to experience anticipatory worry about sleep loss, which paradoxically increases arousal and makes falling asleep even harder.
Quiet Amplifies Ruminative Thinking
As external stimuli diminish at night, your brain shifts into an introspective mode where internal thoughts command full attention. Without daytime distractions, you become acutely aware of unresolved concerns, greatly amplifying worry patterns. Quiet environments heighten cognitive focus on mental chatter, fragmenting thought processes into racing anxieties.
| Nighttime Condition | Cognitive Response |
|---|---|
| Reduced sensory input | Intrusive thoughts intensify |
| Minimal auditory competition | Rumination deepens |
| Silence and solitude | Emotional stress escalates |
| Absence of external cues | Racing thoughts accelerate |
| Quiet darkness | Worry dominates attention |
This neurobiological shift occurs because silence removes cognitive competition. Your sympathetic nervous system activates without distraction buffering, elevating stress hormones and sustaining mental preoccupation. Consequently, emotional rumination increases considerably during quiet periods, perpetuating the anxiety-insomnia cycle. Understanding this mechanism clarifies why nighttime quiet paradoxically triggers heightened worry rather than restfulness.
Conditioned Arousal at Bedtime
Why does your bed, a place meant for rest, trigger alertness instead? Through repeated pairing of time in bed with wakefulness, your brain conditions the bedroom environment to automatically elicit arousal rather than sleep. Sleep-related cues, the bed itself, darkness, lying down, become conditioned stimuli that activate your nervous system at night.
This conditioned arousal resembles sustained alertness rather than acute panic, and it precedes cognitive arousal like worry and rumination. Once established, the pattern becomes self-reinforcing: each night spent awake in bed strengthens the arousal response to bedtime cues. Avoidance behaviors paradoxically worsen this cycle, increasing time awake in bed on subsequent nights and deepening the conditioned fear of sleep itself. This interaction creates a vicious cycle where the initial fear of not being able to sleep intensifies, leading to heightened sleep anxiety and its effects on overall well-being. The longer this cycle continues, the more ingrained the patterns of avoidance and arousal become, diminishing the ability to relax at bedtime.
Anticipatory Sleep-Related Worry
Many people experience excessive, future-oriented worry focused specifically on sleep failure, a cognitive pattern known as anticipatory sleep-related worry. As external distractions fade at night, you’re left with amplified internal focus on your thoughts and bodily sensations.
Your brain’s natural evening arousal shifts, combined with the quiet, dark environment, create ideal conditions for worry to intensify. You likely fixate on “what if” scenarios: What if sleep doesn’t come? What if tomorrow suffers? This rumination window strengthens catastrophic thinking about sleep consequences.
Proximity to the upcoming day fuels performance-related anxiety, while heightened sensitivity to the clock and minor sleep disruptions reinforces beliefs that sleep is failing. This selective attention perpetuates the worry cycle, trapping you in anticipatory anxiety before you’ve even attempted sleep.
Who Is Most Vulnerable to Nighttime Anxiety
Certain populations experience nighttime anxiety at disproportionately higher rates than others, with research consistently demonstrating that vulnerability isn’t randomly distributed across demographics. Women face substantially higher insomnia risk than men, though men experience sharper anxiety increases with shorter sleep durations.
Younger adults aged 18-25 show the largest anxiety increases over the past decade, while older adults demonstrate greater vulnerability to sleep-anxiety effects due to declining sleep quality. Racial and ethnic minorities exhibit stronger associations between short sleep and anxiety compared to non-Hispanic whites.
Socioeconomic status plays a critical role, individuals from lower-income backgrounds report higher sleep disturbances and anxiety, particularly during periods of heightened stress. Marital status also influences vulnerability, with married individuals showing stronger short sleep-anxiety links while unmarried individuals face amplified risks with longer sleep durations.
How Poor Sleep Compounds Anxiety the Next Day
When you’ve tossed and turned through the night, you’re not simply tired the next day, you’re neurologically primed for anxiety. Even losing just one or two hours of sleep elevates your next-day anxiety symptoms, including increased worrying and physiological arousal like rapid heart rate. Sleep loss impairs your brain’s stress regulation systems, lowering your threshold for anxious responses.
Simultaneously, poor sleep reduces positive emotions that normally buffer against anxiety, leaving you emotionally vulnerable. Your cognitive abilities suffer too: attention, working memory, and executive function decline, making it harder to control intrusive worried thoughts. These cognitive deficits often trigger maladaptive thinking patterns, catastrophizing and rumination, that further fuel anxiety. This creates a compounding effect where your sleep deprivation directly intensifies anxiety the following day.
Breaking the Pattern: Understanding Sleep-Related Worry
The anxiety-sleep cycle you’re caught in doesn’t emerge randomly, it’s sustained by specific cognitive and behavioral patterns that you can learn to recognize and interrupt. Research shows that worry, selective attention, and safety behaviors maintain your nighttime distress.
| Pattern | Mechanism | Impact |
|---|---|---|
| Worry | Triggers arousal; 10% higher odds of incident insomnia | Perpetuates cognitive activation |
| Selective Attention | Monitors for sleep threats; heightens worry | Amplifies threat perception |
| Safety Behaviors | Maladaptive habits triggered by unhelpful beliefs | Increases insomnia risk by 7% |
Your brain learns to associate bed with threat rather than rest. When you decrease selective attention and reduce safety behaviors over time, remission becomes possible. Understanding these interconnected processes, how worry maintains arousal while monitoring sustains vigilance, empowers you to target interventions effectively and break the cycle.
Restoring Emotional Balance Through Better Sleep
Breaking free from the anxiety-sleep cycle requires understanding how sleep directly restores your emotional capacity. During REM sleep, your brain resets adrenergic activity in limbic and prefrontal networks, reducing emotional charge from memories while preserving factual content. This neurobiological process recalibrates your emotional sensitivity and strengthens regulatory control over your amygdala, the brain region that amplifies anxiety responses.
When you sleep insufficiently, your prefrontal cortex weakens its regulatory grip on limbic regions, intensifying emotional volatility and nighttime worry. Conversely, adequate high-quality sleep stabilizes mood and increases your resilience to stressors. You’ll notice improved next-day emotional adjustment and reduced anxiety reactivity when you prioritize sleep duration and continuity. By restoring sleep quality, you actively rebuild the neural mechanisms that govern emotional balance and break the vicious cycle perpetuating nighttime anxiety.
Frequently Asked Questions
What Specific Relaxation Techniques Can I Use Right Before Bed to Reduce Nighttime Anxiety?
You can use several evidence-based techniques right before bed. Try 4-7-8 breathing, inhale for 4 seconds, hold for 7, exhale for 8, repeated four times, to calm racing thoughts. Progressive muscle relaxation works well too: systematically tense and release muscle groups from your toes to face over 10, 20 minutes. You’ll also benefit from guided body-scan meditation or imagery of calming scenes using sensory details. Combining these approaches amplifies their effectiveness for reducing nighttime anxiety.
How Long Does It Typically Take to Break the Anxiety-Insomnia Cycle With Proper Intervention?
You’ll typically see improvements within 6-8 weeks using cognitive-behavioral therapy for insomnia (CBT-I). Most patients experience reduced sleep onset time and increased total sleep within this timeframe, with 70-80% showing meaningful gains. However, you’ll need to address both sleep and anxiety simultaneously, as they’re bidirectionally linked. Individual responses vary based on anxiety severity and treatment adherence. You shouldn’t expect overnight results, but consistent intervention breaks the cycle effectively.
Are There Dietary or Lifestyle Changes That Specifically Target Nighttime Anxiety Symptoms?
You can directly target nighttime anxiety through strategic dietary and lifestyle shifts. Adopt a Mediterranean-style diet rich in fiber to reduce inflammation and stabilize cortisol. Eliminate sugar-sweetened beverages and processed foods that disrupt sleep quality. Time your largest meals earlier in the day, finish eating by 8 PM to align circadian rhythms. Limit caffeine after 2 PM. Maintain consistent meal schedules matching your natural chronotype. These evidence-based changes address the physiological mechanisms driving your evening anxiety.
Should I Avoid Napping During the Day if I Experience Nighttime Anxiety Regularly?
Yes, you should generally avoid napping if you experience regular nighttime anxiety. Daytime naps reduce your sleep drive, making it harder to fall asleep at night and disrupting sleep continuity. Long or late-afternoon naps are particularly problematic, they can worsen insomnia and increase anxiety about sleep itself. If you’re struggling with nighttime anxiety, behavioral sleep medicine protocols recommend eliminating naps during treatment to consolidate your nighttime sleep and build stronger evening sleepiness.
When Should I Seek Professional Help for Nighttime Anxiety Rather Than Self-Managing?
You should seek professional help if you’re experiencing persistent insomnia three or more nights weekly for over three months, intense panic attacks at night, or escalating anxiety despite consistent self-management efforts. You’d also benefit from professional support if nighttime anxiety impairs your daytime functioning, causes emotional instability, or you’re relying on substances to cope. Additionally, if you’re experiencing trauma-related symptoms, severe sleep fear, or thoughts of self-harm, don’t delay, contact a mental health specialist immediately.